Advertisement
Word To Pediatricians: IUDs And Implants Top Choices For Teen Birth Control
By Veronica Thomas
Guest contributor
When a teen girl tells her pediatrician she’s thinking about having sex, the response is often a brief talk about abstinence, a handful of condoms, and a referral to the family planning clinic across town.
But a new recommendation makes pediatricians likelier to discuss the whole gamut of birth control methods—with IUDs and hormonal implants topping the list.
Released today by the American Academy of Pediatrics, the recommendation says doctors should discuss a broad range of birth control options with sexually active teens, but should start with the methods that protect against pregnancy best: long-acting reversible contraceptives, which include the hormonal implant, copper IUD and two hormonal IUDs.
Teen pregnancy rates have dropped dramatically over the past two decades to a record low, but the U.S. still has one of the highest rates among developed countries: more than 750,000 pregnancies each year. Though most sexually active teens use some form of birth control, they rarely pick the most effective methods and often use them incorrectly—whether it’s missing a few doses of the pill or accidentally tearing a condom.
"It’s sort of a set-and-forget method."
Heather Boonstra, Guttmacher Institute
Because IUDs and implants don’t rely on any action from the user, they’re a particularly good fit for teens, says Heather Boonstra, Director of Public Policy at the Guttmacher Institute.
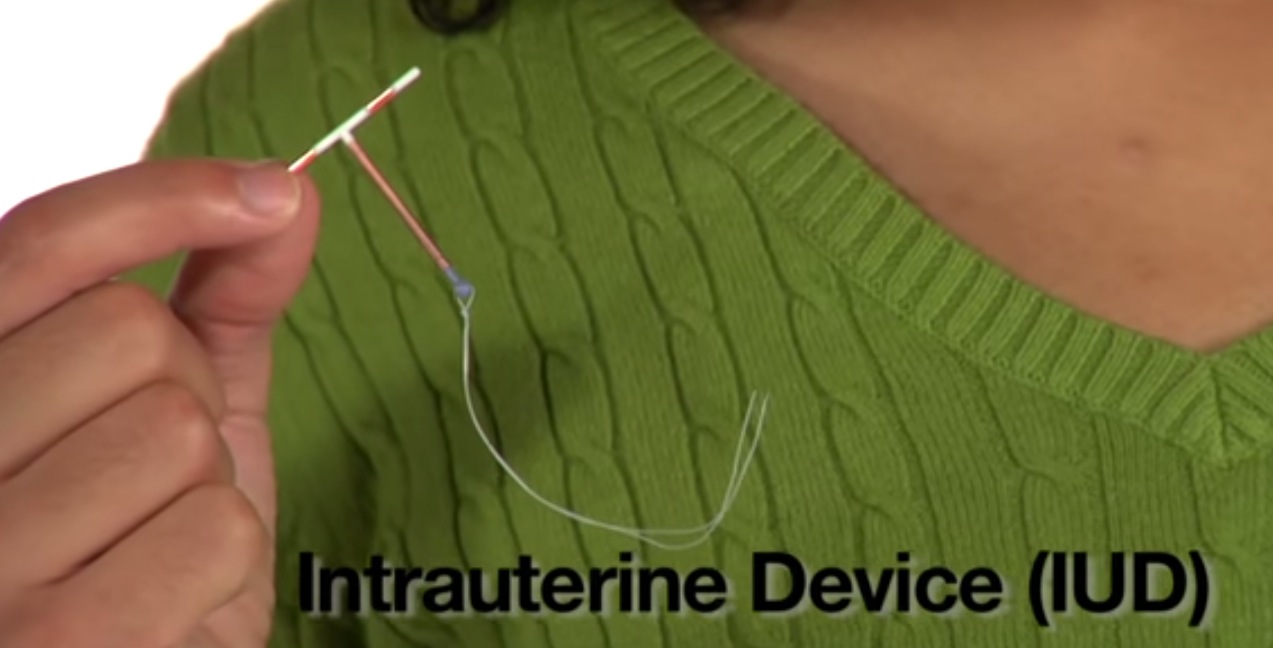
“It’s sort of a set-and-forget method,” she says. Once inserted by a trained professional, an implant or IUD can last from three to ten years, and will be over 99 percent effective. The implant is a matchstick-sized rod inserted in the upper arm; the IUD is a small, T-shaped device placed into the uterus.
Their use has been rising for years in the general population. From 2002 to 2009, implant and IUD use nearly doubled among women overall. But while use of these long-acting methods has also been increasing among teens, less than five percent of all teen contraceptive users currently choose them.
That’s because most teens have never even heard of the implant or IUD, says Boonstra.
“Providers have to recognize that they’re beginning with an audience that is brand new to this whole thing, and that they may have to really guide them through conceptualizing what this method would mean for them,” Boonstra says. “You’re really beginning with ground zero.”
Long-acting reversible contraceptives "are important tools in adolescent pregnancy prevention and assuring the continuation of that decline,” say Dr. Mary Ott and Dr. Gina Sucato, authors of the American Academy of Pediatrics report, in a joint email.
Despite their advantages, IUDs haven’t always been so popular. Their image was long tainted by the 1970’s debacle of the Dalkon Shield—an IUD that caused pelvic inflammatory disease in many women.
But the design flaw at fault has been fixed and tested for decades, Boonstra says. And the IUDs and implant on the market today have over ten years of data supporting their effectiveness and safety for teens, the American Academy of Pediatrics report says.
That’s why the Academy aims to increase the availability and use of long-acting reversible contraceptives. And its statement is just the latest of these efforts. The American Congress of Obstetricians and Gynecologists has been promoting IUDs and implants for teens since 2007, and the CDC released similar recommendations last year.
The teens who have heard about the long-acting methods are often nervous about the pain, negative side effects, or having a foreign object placed in their bodies. These concerns aren’t unfounded. According to the Academy report, more than half of teens report moderate to severe pain during the insertion of IUDs, and there may be some abnormal bleeding in the first few months.
Though comparable to the pill’s cost over the long run, long-acting methods have a steep up-front cost ranging from $500 to $1,000—a price tag that has deterred teens in the past. But now, with the passage of the Affordable Care Act, insurance plans are required to cover contraception with no additional cost to the patient. “Hopefully, cost is melting away as a barrier, with the ACA,” Boonstra says.
But even with this increased access and the improved image of long-acting methods, some myths and hesitation still linger. "Hopefully with the AAP coming out with this statement, some of that will be dispelled and people will get more comfortable with the notion of [them] as a really good first-line contraception option," says Dr. Sarah Pitts, an adolescent health specialist at Boston Children's Hospital. That’s why counseling by pediatricians is key, she says.
"Parents and families are concerned about the safety of their adolescents."
Dr. Mary Ott and Dr. Gina Sucato, AAP
"Parents and families are concerned about the safety of their adolescents," write Dr. Ott and Dr. Sucato in a joint email. "It will be important to remind them that the current [long-acting reversible contraceptives] on the market are all safer than pregnancy."
In addition to discussing potential benefits and drawbacks of long-acting methods, the Academy states that pediatricians should ensure access to these devices—whether through their own office or by referring to others.
“Pediatricians are all over the map,” Dr. Ott says. Some practices might have one clinician who is trained in inserting implants and IUDS, while others may have to refer patients out to adolescent health specialists, gynecologists or family planning clinics.
Dr. Pitts worries this referral system might be a hurdle in getting IUDs and implants to the teens who want them. “If a pediatrician has [birth control] pills that they can give away in their office confidentially, versus a seventeen-year-old who’s trying to figure out how to get to an adult facility to get an IUD placed, they’re going to be more likely to give them a pack of pills and say, ‘Let’s do this first and see how it goes,’” she says. But that may not always be the best choice, since teens are likely to miss doses or stop taking the pill all together.
To avoid these gaps in pregnancy protection, the Academy report encourages pediatricians to frequently follow up with their patients and help them continue and adhere to the contraceptives they choose.
“Most pediatricians screen for sexual behavior, are generally trusted by adolescents, and are often the first providers that adolescents disclose to,” says Dr. Ott. Often, they also have a long-term relationship with the teen and family, and are thus more able to discuss sensitive issues.
So will these new recommendations actually lead to a big jump in IUDs and implants among teens?
“I think it’s very likely that all of these efforts will show an increase in [long-acting reversible contraceptive] use over time, and that’s important,” says Boonstra. “At the same time, what’s most important is that adolescents are counseled and are given enough information to think about what method is best for them.”