Advertisement
10 Things To Know About This Flu Season, Starting With No. 1: It's Not Even Over

If you were felled by the flu recently and left asking for the license plate of the Mack truck that hit you, here it is: A/H3N2. That has been the dominant flu strain this season, and while none of the strains are nice, this one can give new meaning to nasty.
"This has been a pretty average H3N2 year — those do tend to be more severe," says Centers for Disease Control flu tracker Lynnette Brammer.
Tens of thousands of Americans die from the flu each year, on average. This season, the CDC reports 55 flu-linked deaths in children so far, and older people have been particularly hard-hit, though their mortality numbers are not yet in.
Among my friends and colleagues, I've been hearing chest-rending coughs for weeks; tales of flu-sparked ear infections and lung infections and sinus infections; complaints that recovery from a flat-on-back-can't-even-watch-TV state to any semblance of normal can take not days but weeks.
Misery stokes curiosity, so I turned to Dr. Marty Hirsch. An infectious disease specialist and virologist at Massachusetts General Hospital since 1969, he's coming up on a half-century in the flu trenches. He's also a great explainer. Here's what he told me, distilled into 10 lessons:
1. It ain't over til it's over, and it ain't over.
"Influenza season peaked a few weeks ago but it's still widespread. That means if you haven't gotten the vaccine yet, it's still not too late to get it. And it's a wise choice to make because you're not out of the woods yet."
(In fact, CDC statistics show that while H3N2 is declining, a second wave of "B" flu has been going strong in recent weeks.)
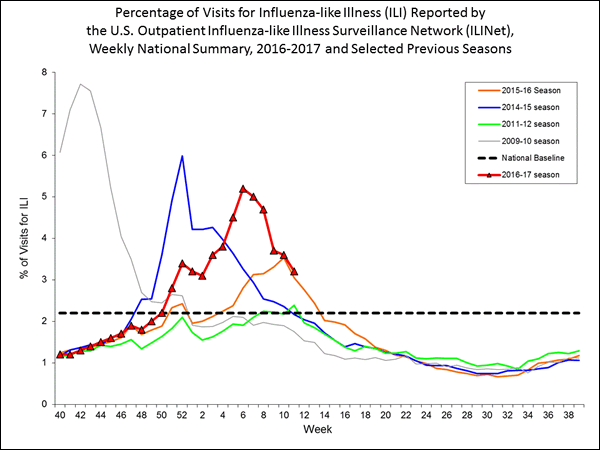
2. It's not just me: This really is a pretty bad flu year.
"There are several different types of influenza viruses that circulate, and whenever the A virus type H3N2 circulates, there are particularly severe cases in lots of people. That's what's happening this year.
"We had the same kind of situation back in 2012-'13. In other years, other influenza viruses predominate, like H1N1 or the B viruses — they tend to be milder years. So I think you are correct that this is a bad year."
3. And especially bad for old folks and little ones.
I asked Dr. Hirsch about my sense that there had been more public concern — bordering on panic — when H1N1 hit back in 2009.
"That's right. When H1N1 came along in 2009, it was a novel strain. We hadn't seen it in many, many decades, and thus very few people — particularly the younger people — had any immunity. When a new pandemic strain develops, it tends to affect the very young, and can cause severe, even fatal, disease.
"The usual years we have — like we're having this year — these viruses have been around for a while. So the major targets are those individuals over the age of 65, as well as the very young children under the age of four who had never seen this virus before."
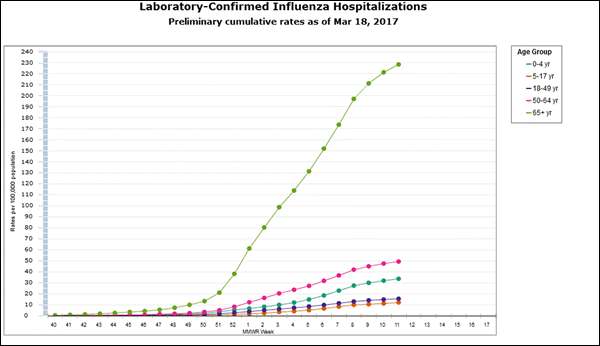
4. Elders are more vulnerable because immune systems age.
"People generally tend to lose some immune function over time. In addition, the over-65 crowd often has other underlying co-morbidities like diabetes or cancer or some kind of immuno-compromising disorder. So whenever you have someone with somewhat of a diminished immune system, the virus gets a foothold and can replicate much more than someone whose immune system is intact, and that tends to be the case with the over-65 population. So the vast majority of hospitalizations, and the vast majority of influenza-associated deaths, occur in the over-65 population."
5. And we don't really know why this bug is so mean.
"We don't fully understand why that's the case. It has a hemagglutinin — that's the 'H' part of the virus --
that tends to be more virulent or more pathogenic than the hemagglutinin of some other viruses. Exactly why that's the case, we don't know.
"In addition, the vaccines that we do produce seem to be less effective against the H3 virus than they are against other ones. From the CDC data this year, the vaccine seems to be effective overall in about 48 percent of the population. But if you look at the different subtypes, it's 73 percent effective against the B virus, and only 43 percent against the H3N2 virus, so the cards are sort of stacked against [people who get] the H3N2 virus."
6. Flu doesn't kill people (usually), it opens the door to killer bacteria.
When a loved one is sick, I tend to get most scared after several days have passed and there's no improvement, or even a worsening. I asked Dr. Hirsch if it was correct that what's scariest is not the virus itself but the bacterial infection it may unleash within days.
"That certainly is correct. And if you go back to the major pandemics like the one we had in 1918, it's usually deaths caused by bacterial super-infection — and usually pneumonia, that is caused by staphylococcus or pneumococcus or other organisms that are, as you say, unleashed during influenza virus infections. Influenza itself can kill individuals but does it very rarely.
"What appears to occur is a couple of things: Influenza itself can help suppress the immune response to other agents, like the pneumococcus or the staphylococcus. In addition, it affects the respiratory cells — what we call the epithelial cells, in the respiratory tract, and opens up gaps where these bacteria can enter. So partial destruction of the respiratory tract epithelium allows these other organisms to take hold and grow.
"These viruses attack cells, and they can destroy cells. And thus, the usual barriers to the bacterial organisms aren't there any more, so they can get underneath the epithelium or underneath the 'skin,' as you might say, of the respiratory tract and grow in spots where they don't ordinarily grow, and then they can get down into the lungs. And that, combined with the virus suppressing the host immune response to the organisms, allows the organisms to take hold."
7. BTW, if flu doesn't get you, other viruses might.
"Flu does a good job of wrecking up the respiratory tract. There are other viruses that we call parainfluenza virus or RSV that can do the same kinds of things. And in years when the influenza virus is particularly mild, some of these other viruses can do the same thing.
"During the years that influenza vaccine partially protects people against influenza itself, other viruses may fill the gaps. So sometimes, even when we have a good vaccine match, it doesn't necessarily mean that respiratory disease is going to be less that year."
8. Better, then suddenly worse? Watch out.
More reassurance from Dr. Hirsch that I'm not crazy when I start getting scared several days in, when the patient had seemed better but then took a turn for the worse:
"We learn in medical school that there are different patterns during influenza. One day after another of severe disease — that's usually the result of the virus itself. But the picture you paint — the illness starts to get better and suddenly gets a lot worse, fever spikes up, and the patient starts coughing and producing sputum — that's a telltale sign that a bacterium has taken over and that we'd better start treating the bacteria as well.
"You shouldn't treat everybody with influenza with antibiotics; that will do more harm than good. But if you see that pattern, where you get an initial improvement and then a sudden worsening, that's a sign that you better look for bacteria."
9. And bad flu years mean more bacterial infections.
"The worst epidemic we've ever had was 1918. Back then, we didn't have the antibiotics, and that was when all of these different patterns were described. The vast majority of people who died during the Spanish flu back in 1918 died of bacterial infections rather than viral infection.
"Those patterns still hold. I think it's a mistake for physicians to prescribe antibiotics to somebody who has the characteristic flu. We do have anti-flu drugs like Tamiflu that have some effect, and it's certainly reasonable to give those drugs. But you should hold the antibiotics until you really have signs that bacteria has hit the scene."
10. If it's taking a long time to fully recover, it's not just you.
"It's a damaging virus, and it takes the host epithelial cells in the respiratory tract time to recover. That's why coughs often persist for weeks at a time. And the malaise and fatigue vary greatly from individual to individual — some can recover in a week or two, others take many weeks before they recover. That's often related to age and other underlying conditions that predispose you to a long recovery.
"So don't be surprised, and be positive it will eventually get better. Also, getting a vaccine helps shorten the subsequent recovery period, because the virus replicates to a lower degree, and thus the course of the infection should be shorter, if you've been previously immunized against that particular strain of virus."
Readers, did it get you this year? How bad was it?
