Advertisement
With Health Reform, An Increased Demand For Safety-Net Hospitals, Study Finds
It's always good to get an outsider's perspective.
So, with that in mind, here's a new study with findings that are no surprise to health policy types in Massachusetts, but may be notable to everyone else, including the researchers from Washington, D.C. and elsewhere who carried out the analysis. Published today in the Archives of Internal Medicine, the study found that even after the Massachusetts health reform law and a spike in the number of people with health insurance, patients still chose to get care at safety-net hospitals and community health centers. Most people surveyed said they continued to seek care at these hospitals and health centers because they were convenient and affordable or provided important, non-medical services.
The study concludes: “Despite the significant reduction in uninsurance levels in Massachusetts that occurred with health care reform, the demand for care at safety-net facilities continues to rise...Most safety-net patients do not view these facilities as providers of last resort; rather, they prefer the types of care that are offered there. It will continue to be important to support safety-net providers, even after health care reform programs are established.”
Study author Leighton Ku, Ph.D., M.P.H., from George Washington University, Washington, D.C., explains that some people thought that once patients got an insurance card, they'd flee the safety-net hospitals. "You might think that the newly insured would choose to go to the MGHs not the Boston Medical Centers, the private doctors in Back Bay, not the community health centers...but that is not what we found."
Indeed, for Robert Seifert, Principal Associate at the Center for Health Law and Economics at the University of Massachusetts Medical School, the results of the study come as no surprise. He sent me this note: "The so-called safety net providers have long served the medical and non-medical needs of low-income, formerly uninsured patients and they continue to do so. They are part of the communities in which they operate, and the transportation, language interpretation and other services they provide make accessing their services both possible and comfortable. The patients have changed only their insurance status; their other needs remain, and many continue to see the community health centers and safety net hospitals as their best option for meeting those needs. They are, in effect, a medical home to many, and gaining insurance has not changed that."
WBUR's Martha Bebinger, who was in the thick of covering health reform back in 2006 (and remains so) said from her perspective, the study ranks rather high on the "duh" scale. She said the Massachusetts health reform law was set up with all kinds of subsidies and incentives to funnel newly insured patients to safety net hospitals, where, for instance, they could get the only Somali translator in the city, and other specialized services. She sent me this email:
The state law tried to make sure that [uninsured] patients who had been getting care at community health centers and safety net hospitals would continue to do so, and this study suggests that those efforts worked. Under the law, residents who qualified for free or subsidized coverage had a choice of four insurance options, three of which were run by or affiliated with the health care safety network. These four plans were the only option for subsidized coverage during the first three years of the law. So, by design, if low and moderate income patients wanted care, they went to a safety net hospital or community health center
Still, the study findings are worth noting:
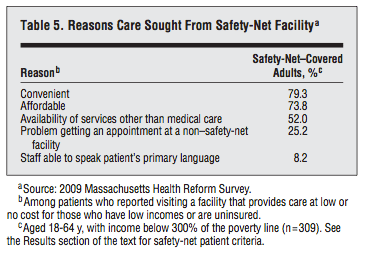
Between calendar years 2005 and 2009, the number of patients receiving care at Massachusetts CHCs increased by 31.0%, and the share of CHC patients who were uninsured fell from 35.5% to 19.9%. Nonemergency ambulatory care visits to clinics of safety-net hospitals grew twice as fast as visits to non–safety-net hospitals from 2006 to 2009. The number of inpatient admissions was comparable for safety-net and non–safety-net hospitals. Most safety-net patients reported that they used these facilities because they were convenient (79.3%) and affordable (73.8%); only 25.2% reported having had problems getting appointments elsewhere.
(Safety-net hospitals were defined as those that in 2009 received 20 percent or more of their net patient service revenue from Medicaid or two state programs for low-income patients: Commonwealth Care and the Health Safety Net program. Of course, Boston Medical Center and Cambridge Health Alliance are the major safety-nets here, with nearly 50% of patient revenue from these subsidized programs. But as part of the study, authors identified 17 institutions as safety-net hospitals and 48 without that designation.)
Ku said the study (funded by Blue Cross Blue Shield of Massachusetts Foundation) offers some insight for the nation. "Massachusetts is an imported harbinger for the rest of the country, an advanced signal, " he said. The takeaway here is that "we need to remember that the safety-net system is important and brings services that the consumer wants." On the other hand, he said, the research also serves as "a warning" to safety-net providers. "The fact that people are still coming to them doesn't mean that will be the case everywhere. If they [the hospitals] are not offering good services and making patients happy, once people have insurance, they might walk away."
Indeed, in an accompanying editorial, Mitchell H. Katz, M.D., from the Los Angeles County Department of Health Services says:
“The important lesson from Massachusetts is that the newly insured continued to seek care in the safety net... However, this scenario may differ in other parts of the country, depending on perceived quality and convenience of safety-net providers and the degree of competition from other providers."
He adds: “Ironically, safety-net providers have more experience working in teams than most commercial providers because low reimbursement rates have forced them to learn to be more cost-efficient...The challenge will be proving that they can also be a system of choice for their patients, not just in Massachusetts, but across the country.”
This program aired on August 8, 2011. The audio for this program is not available.
