Advertisement
10 Scary Reasons To Fight Obesity Before Pregnancy

Please forgive the piling on. There's already enough pressure to lose poundage if you're obese. And pregnant women already have plenty of worries, inflamed by crazymaking compilations of all that could go wrong like "What To Expect When You're Expecting."
But talk to the researchers at MIRI, Tufts Medical Center's Mother Infant Research Institute, and you come away bowled over by all the powerful reasons to aim for a normal weight before pregnancy.
It turns out that obesity in pregnant women heightens risks in ways that you might never suspect: It increases the chances of stillbirths, birth defects, infections, even pediatric asthma — and the list goes on.
You also learn from the MIRI researchers that even if you do enter pregnancy obese, you can still make a difference by watching your weight during those critical months.
Doctors have long focused on women's weight gain during pregnancy. But recent research has clarified the importance of a woman's weight upon entering pregnancy as well, said Dr. Sarbattama Sen, a Tufts Medical Center neonatologist and researcher. "As time has gone on," she said, "it's become more and more clear that so many of the forces that are affecting fetal health are being exerted very early in pregnancy, before women even know they're pregnant."
At the same time, the obesity epidemic has spread, as well. At Tufts Medical Center, as at many hospitals, one in every five pregnant patients these days is obese — not just overweight, but obese — and the obstetrics department has had to add new beds made for larger mothers.

Dr. Errol Norwitz, the hospital's chief of obstetrics and gynecology, offers these first five reasons to lose weight before pregnancy, based mainly on risks to the mother's own health; then Dr. Sen will add five focused more on the baby.
1. The most dangerous complications of pregnancy, the life-threatening ones, are far more common in obese women.
The two medical complications that are highest risk to the mother are blood clots in the legs that go to the lungs, and a condition called pre-eclampsia. They account for nearly 40 percent of all maternal deaths during pregnancy, and both are much more common in obese women.
Pre-eclampsia, for example, occurs in 5-8% of women overall, but 15-24% of morbidly obese women (those with a Body Mass Index over 40.) And as with many of these risks, there does appear to be a "dose effect:" the more obese you are, the higher the risk. Deaths are still exceedingly rare, but the danger does rise.
2. The risk of stillbirth also triples in morbidly obese women.
Women who are obese tend to have a harder time with conception and are also more likely to miscarry, even if the baby is conceived through IVF. And morbidly obese women are almost three times more likely than non-obese women to have a full-term stillbirth, for reasons that aren't entirely clear.
[module align="left" width="half" type="pull-quote"]"Each one of us as a fetus goes through more developmental milestones in utero than we ever will once we're born."[/module]
It may be more difficult to test the babies in obese women, or it could be connected to other medical problems. Women with morbid obesity tend to also have other conditions, from diabetes and high blood pressure to asthma and sleep apnea. Other theories involve the immune system and hormones.
Overall, the risk of unexplained full-term stillbirth is about 1 in 2,000; in morbidly obese women it's more like 1 in 600.
3.Cesarean sections are not only more common in obese women, but more dangerous.<
The overall Cesarean-section rate is about one-third of deliveries; in obese women it's more like one half.
In an obese woman who has a Cesarean, the risks of complications from anesthesia are much higher because of airway problems. It's harder to get an epidural in; there tends to be more blood loss and much more infection; and again, obese women are more likely to get blood clots in their legs.
4. The risk of gestational diabetes or glucose intolerance triples in morbidly obese women.
The overall risk of pregnancy-related diabetes is 5%, but in morbidly obese women it's closer to 15%. If a pregnant woman has gestational diabetes, the risk rises that the fetus will get very big and have delivery problems that could cause injuries.
5. Premature birth is about one-and-a-half times more common in obese women.
Not sudden premature birth, that is, but pre-term delivery because of medical necessity, for reasons mentioned above.

And now from Dr. Sen, the neonatologist, five reasons focused more on the baby.
6. Children born to obese mothers are more likely to become obese adults.
And no, it's not just that the same genes are at work. We know that babies of obese mothers are born heavier, and the heaviness is fat mass. There’s no doubt that the various environmental influences don’t help, but the babies are being born with one strike already against them.
7. Studies link obesity in the mother to asthma in the child.
When I started doing this research about three years ago, there was one study linking maternal obesity to asthma. Now we have five more, and they've conclusively shown that the pre-pregnancy body mass index of a mother is linked to the development of asthma in her children. They show asthma is about 1-1/2 times as likely in the children of obese mothers. These children have higher rates of respiratory illness as early as 1 year of age and higher rates of asthma into their teens.
8. Children born to obese mothers are at higher risk of birth defects.
Though they're generally rare, birth defects are more common when mothers are obese. Babies of obese mothers are 3.5 times more likely to have a neural tube defect and twice as likely to have congenital heart disease. Both have profound consequences for the long-term health of the child.
9.Obesity's effects on immune function can translate into impaired infection-fighting.
Obese pregnant women are less able to fight certain infections compared to non-obese women. Infection can lead to pre-term delivery; also, we know that the inflammation caused by an acute infection during pregnancy can have profound long-term neurological effects on the fetus.
10. Obesity is associated with lower breastfeeding rates, and appears to affect the baby's nutrient levels.
Breastfeeding is an important aspect of infant health. The rate of breastfeeding tends to be lower in obese women, and there are convincing physiological reasons in terms of hormonal differences. Also, researchers are starting to look at indications that maternal obesity influences the levels of micronutrients such as iron and folate not only in the mother but the child as well.
Now for the good news:
"For women who are pregnant and who are obese," Dr. Sen said, "I want to stress that pregnancy is such a critical time, it's not too late to make changes.
[module align="right" width="half" type="pull-quote"]'Women who achieve ideal weight gain during pregnancy are much less likely to have long-term complications, both in themselves and in their babies.'[/module]
We know that obese women who don't gain as much weight during pregnancy do better in terms of pregnancy outcomes than obese women who gain too much. Women who achieve ideal weight gain during pregnancy are much less likely to have long-term complications, both in themselves and in their babies. It's an ideal opportunity to make the lifestyle modifications needed."
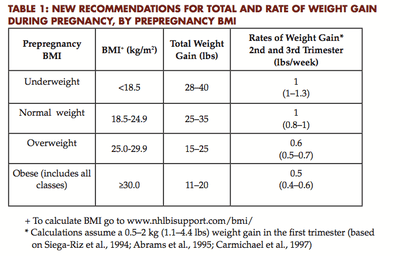
The Institute of Medicine's recommendations for weight gain during pregnancy are here, and here's the basic chart:
And if it's too late for this pregnancy, there's always the next one. Dr. Norwitz said that turning patients' focus to pre-pregnancy weight can be logistically difficult given that most American pregnancies are unplanned. Instead, he said, it may make more sense to focus on the "inter-pregnancy interval."
"From the moment you deliver your previous child," he said, "you have to improve your lifestyle: eating better, exercising, stopping smoking and drug use, maintaining adequate weight control. It's the same message, but what I've found is that if you focus on the so-called inter-pregnancy interval, you're more likely to be successful. It's more logistical than anything."
Here's a particularly inspiring concept from Dr. Norwitz: "Each one of us as a fetus goes through more developmental milestones in utero than we ever will once we're born."
And according to a fascinating line of research known as the Barker Hypothesis, which explores in-utero changes in gene expression, what happens in your uterus could affect not just your baby but your baby's babies as well. It could make quite a Post-It on a pregnant woman's refrigerator door: "Think about your grandchildren."
This program aired on November 18, 2011. The audio for this program is not available.
