Advertisement
Sudden-Onset OCD In Kids: Possible Causes Broadened, Trial Ongoing
It's an odd and terrifying phenomenon: Seemingly overnight, a child begins to show extreme symptoms of Obsessive Compulsive Disorder and nerve trouble, from tics to excessive fears.
A hypothesis, controversial but long gathering steam, proposes that this sudden-onset syndrome could be the result of a strep infection, which triggers antibodies that mistakenly attack part of the brain. The syndrome was originally called PANDAS, or Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infection — but has now been broadened beyond strep to PANS, or Pediatric Acute-onset Neuropsychiatric Syndrome. Federal research authorities have just put out a release (below) describing the state of the scientific consensus on PANS and a clinical trial using immune-based therapy now under way.
I wrote about PANDAS way back in 2003 for the Boston Globe. The story began:
KENNEBUNKPORT, Maine - Sammy Jelin, math whiz and natural comedian, sailed through fifth grade, a school enthusiast eager for the bus each morning. By the start of sixth grade last fall, he could barely make it to school at all: In just weeks, his world had turned into a minefield of germ phobias, invisible walls, and constant tics - hallmarks of obsessive compulsive disorder and Tourette's syndrome.
By this May, Sammy's mother, Beth Jelin, was nearing her wits' end. Then an acquaintance mentioned that her son had contracted similar mental ailments through a streptococcus infection. The idea sounded wild, especially because Sammy had never had strep throat. But a prompt blood test did turn up unusually high levels of strep, and Sammy went on antibiotics.
Within days, Sammy got so much better that Beth Jelin is convinced that undiagnosed strep was the culprit, and a growing body of research, though still controversial, suggests she might be right.
It's interesting to see how far the field has come in nearly a decade. Here's the full, nicely done release from the National Institute of Mental Health:
Possible causes of sudden onset OCD in kids broadened
NIH immune-based treatment study underwayCriteria for a broadened syndrome of acute onset obsessive compulsive disorder (OCD) have been proposed by a National Institutes of Health scientist and her colleagues. The syndrome, Pediatric Acute-onset Neuropsychiatric Syndrome (PANS), includes children and teens that suddenly develop on-again/off-again OCD symptoms or abnormal eating behaviors, along with other psychiatric symptoms – without any known cause.
PANS expands on Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcus (PANDAS), which is limited to a subset of cases traceable to an autoimmune process triggered by a strep infection. A clinical trial testing an immune-based treatment for PANDAS is currently underway at NIH and Yale University (see below).
“Parents will describe children with PANS as overcome by a ‘ferocious’ onset of obsessive thoughts, compulsive rituals and overwhelming fears ,” said Susan Swedo, M.D., of the NIH’s National Institute of Mental Health (NIMH), who first characterized PANDAS two decades ago. “Clinicians should consider PANS when children or adolescents present with such acute-onset of OCD or eating restrictions in the absence of a clear link to strep.”
Swedo, James Leckman, M.D., of Yale University, and Noel Rose, M.D., Ph.D. of Johns Hopkins University, propose working criteria for PANS in February 2012 in the open source journal Pediatrics & Therapeutics.
“As the field moves toward agreement on this broadened syndrome, affected youth will be more likely to receive appropriate care, regardless of whether they are seen by a neurologist, pediatrician or child psychiatrist,” said NIMH Director Thomas R. Insel, M.D.
Differing causes sharing a “common presentation”
The PANS criteria grew out of a PANDAS workshop convened at NIH in July 2010, by the NIMH Pediatric and Developmental Neuroscience Branch, which Swedo heads. It brought together a broad range of researchers, clinicians and advocates. The participants considered all cases of acute-onset OCD, regardless of potential cause.
Clinicians reported that evaluations of more than 400 youth diagnosed with PANDAS confirmed that affected boys outnumbered girls 2:1, with psychiatric symptoms, always including OCD, usually beginning before 8 years.
Although debate continues about the fine points, the field is now of one mind on the core concept of “acute and dramatic” onset of a constellation of psychiatric symptoms. There is also broad agreement on the need for a “centralized registry” that will enable the research community to analyze evidence from studies that will eventually pinpoint causes and treatments. Such a registry is currently under development by members of the International Obsessive Compulsive Foundation (IOCDF).
Since a diagnosis of PANS implies no specific cause, clinicians will have to evaluate and treat each affected youth on a case-by-case basis.
“PANS will likely turn out to include a number of related disorders with different causes that share a common presentation,” explained Swedo.
The authors propose that a patient must meet 3 diagnostic criteria for a diagnosis of PANS:
1. Abrupt, dramatic onset of OCD or anorexia.
2. Concurrent presence of at least two additional neuropsychiatric symptoms with similarly severe and acute onset. These include: anxiety; mood swings and depression; aggression, irritability and oppositional behaviors; developmental regression; sudden deterioration in school performance or learning abilities; sensory and motor abnormalities; somatic signs and symptoms.
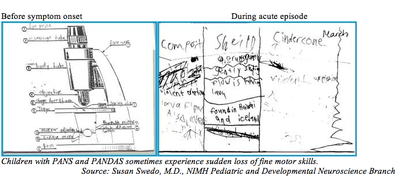
3. Symptoms are unexplainable by a known neurologic or medical disorder.Among the wide range of accompanying symptoms, children may appear terror stricken or suffer extreme separation anxiety, shift from laughter to tears for no apparent reason, or regress to temper tantrums, “baby talk” or bedwetting. In some cases, their handwriting and other fine motor skills worsen dramatically. Leckman’s team at the Yale Child Study Center is in the process of developing assessment tools for diagnosing the syndrome.
PANDAS treatment study targets errant antibodies
Meanwhile, Swedo, Leckman, and Madeleine Cunningham of the University of Oklahoma, and colleagues, are collaborating on a new, multi-site placebo-controlled study, testing the effectiveness of intravenous immunoglobulin (IVIG) for reducing OCD symptoms in children with PANDAS.
Previous human and animal research suggested mechanisms by which strep-triggered antibodies mistakenly attack specific brain circuitry, resulting in obsessional thoughts and compulsive behaviors.
“Strep bacteria has evolved a kind of camouflage to evade detection by the immune system,” Swedo explained. “It does this by displaying molecules on its cell wall that look nearly identical to molecules found in different tissues of the body, including the brain. Eventually, the immune system gets wise to this ‘molecular mimicry,’ recognizes strep as foreign, and produces antibodies against it; but because of the similarities, the antibodies sometimes react not only with the strep, but also with the mimicked molecules in the human host. Such cross-reactive ‘anti-brain’ antibodies can cause OCD, tics, and the other neuropsychiatric symptoms of PANDAS.”
IVIG, a medication derived from normal antibodies, neutralizes such harmful antibodies, restoring normal immune function. It is used to treat other autoimmune illnesses and showed promise in a pilot study with PANDAS patients.
“We predict that IVIG will have striking benefits for OCD and other psychiatric symptoms, and will prove most effective for children who show high levels of anti-brain antibodies when they enter the study,” said Swedo.
Prospective study participants are first screened by phone by investigators at the NIH or the Yale Child Study Center. Those who meet eligibility requirements are then randomized to receive either active IVIG or a placebo procedure during a brief inpatient stay at the NIH Clinical Center. The researchers remain blind to which children received the active medication; after 6 weeks of placebo control, they give any children whose symptoms fail to improve the option to receive open-label active treatment.
In addition to assaying for antibodies that attack brain cells, the researchers use magnetic resonance imaging to see if the treatment reduces inflammation in an area of the brain known as the basal ganglia, which is thought to be the target of the errant antibodies. They also analyze levels of immune system chemical messengers (cytokines) in cerebrospinal fluid and blood – with an eye to identifying biomarkers of disease activity and potential predictors of treatment response.
The study was launched with support from the NIH Clinical Center’s Bench to Bedside program, which encourages such intramural-extramural collaborations in translational science.
This program aired on March 21, 2012. The audio for this program is not available.
