Advertisement
The CEO Checklist For Better Medical Care
The simple concept — that a short, well-crafted list of basic but critical items can help focus even the most accomplished doctor and improve care — was pioneered by Dr. Peter Pronovost, of Johns Hopkins and popularized by Dr. Atul Gawande, the New Yorker writer and surgeon at Brigham & Women's Hospital. Gawande wrote about checklists for surgery, among others. And recently, a study came out on an effective, World Health Organization-backed checklist for childbirth.
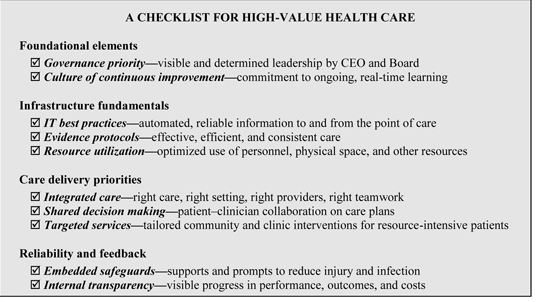
Today, the Institute of Medicine releases a new paper: A CEO Checklist for High-Value Care , written by 11 hospital chiefs, among them Gary Gottlieb, the president and CEO of Partners HealthCare System, Inc.
But a surgical checklist, which includes things like identifying the patient and surgical site and making sure all the sponges are accounted for after an operation, may be simpler and more practical then establishing a "culture of continuous improvement — commitment to ongoing, real-time learning," which is #2 on the CEO's Checklist.
Indeed the IOM paper notes: "The strategies in this Checklist are not, of course, of the “one-and-done” variety. Rather, the items we present here are elements that must become core components of an organization’s DNA."
But if an institution's DNA actually does evolve, care improves, according to these CEOs, and costs decline as certain wasteful practices are eliminated.
For instance, the paper notes two examples involving Partners:
1. Partners HealthCare’s Connected Cardiac Care Program (CCCP) is a home monitoring program for heart failure (HF) patients at risk for hospitalization. CCCP’s core components are care coordination, education, and development of self- management skills through the use of telemonitoring. Patients use home monitoring equipment to submit weight, blood pressure, heart rate, and symptoms on a daily basis.
• Better care: 51 percent reduction in HF hospital readmission; 44 percent reduction in non-HF hospital readmission
• Lower costs: More than $10 million in savings to date ($8,155 per patient)2. Partners participated in a 3-year demonstration project to test strategies to improve the coordination of high-cost Medicare patients. To help primary care physicians manage these patients, case managers were integrated into primary care practices. Case managers developed personal relationships with enrolled patients and worked closely with physicians to help identify gaps in patient care, coordinate providers and services, facilitate communication (especially during transitions), and help educate patients and providers.
• Better care: 20 percent reduction in admissions; 13 percent reduction in ED visits
• Lower costs: $2.65 saved for every $1 spent; 7 percent net savings for each patient in the program
This program aired on June 5, 2012. The audio for this program is not available.
