Advertisement
Narrating Medicine: What I Learned About Cancer Survivorship Clinics
When a friend recently finished her grueling year of breast cancer chemotherapy, she received warm congratulations from her health care team and was invited to ring a special bell set up in her doctor's office. Another friend, cancer-free for a year, is rewarding herself by taking part in a bike ride fundraising for cancer research. Me? Now that I have been on maintenance chemo for two years, I am celebrating by getting a mammogram.
Let me explain. Cancer survivors need continued specialized health care to assess for late side effects from the treatment and the cancer, and specialized preventative care. For example, girls who have received radiation therapy need mammograms at a far younger ages than their peers, and children who have received brain radiation need a yearly hearing assessment.
One way to assess and treat cancer survivors is through Survivorship Clinics. These are places where patients get multidisciplinary appointments and where survivors meet with, for example, specialized health care providers, mental health care providers, nutritionists and physical therapists.
Research presented this week at the American Society of Clinical Oncology describes the value of such clinics. Care of survivors is especially important in children: Over 80 percent of children with cancer survive and need a care plan to guide surveillance for late effects of cancer therapy.
Yet while almost three-quarters of children have a late side effect from their cancer treatment fewer than 20 percent get surveillance for late effects.
In the study presented this week, the authors randomized patients to either attending a Survivorship Clinic or receiving a customized survivorship care plan to use with their primary care provider. The authors found that the participants in the Survivorship Clinic were much more likely to receive recommended testing and more likely to have late effects of treatment identified. In fact, out of about 50 patients in each group, the authors found previously unidentified late effects of cancer — including obesity, high lipids, hypothyroidism, neuropathy, osteopenia, restrictive lung disease, substance abuse and anxiety — 21 times in the Survivorship Clinic group, but only once in the group that that received a written care plan.
The study didn’t explore why the Survivorship Clinics were better. My guess is that it was, in part, because most primary care doctors don’t get trained in long-term care of cancer patients. But I think the bigger benefit of these clinics -- as with multidisciplinary clinics for diabetes and cystic fibrosis and other chronic diseases -- is that having a number of people with varied expertise working together, focusing on one person in one place, is an ideal way to think about a patient. These clinics focus on the whole person, not just on a patient's disease.
To be sure, Survivorship Clinics can be expensive and are usually located only at big hospitals in big cities. And only one-third of cancer survivors go to Survivorship Clinics. Many people don’t want to go to a Survivorship Clinic because it reminds them of their cancer -- of what they’ve survived, and what they might not have survived.
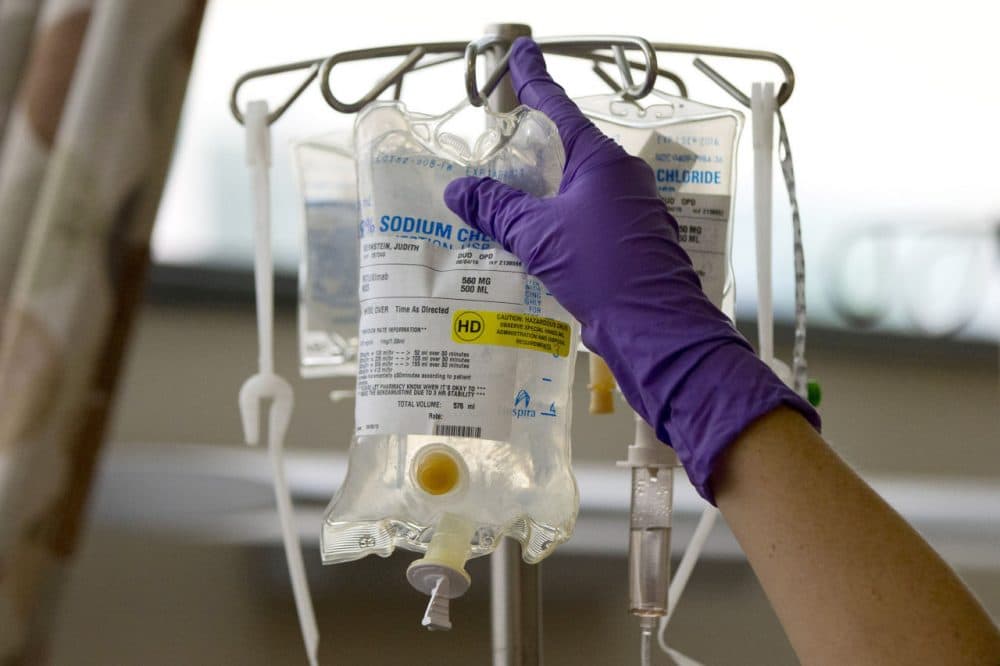
When I was first diagnosed with metastatic colon cancer in 2013, the care plan involved intense chemotherapy — oxaliplatin, bevacizumab, irinotecan and capecitabine — every other week. I was taking prednisone and aprepitant for the nausea, lidocaine cream for the injection site pain and pegfilgrastim for the decreasing white blood cell count. My other regular intake included scrambled eggs, Ensure, meat and white bread. Preventive care — like mammograms, pap smears and regular exercise -- was not part of the care plan.
Last week, two and a half years after my cancer diagnosis and two years after I started maintenance chemotherapy and went back to work, I went to Survivorship Clinic. My doctors didn’t recommend it -- a friend did. My primary care doc and my gynecologist are both great doctors, but when I have asked questions about preventive care related to my cancer (like, "Should I get re-vaccinated?") they both acknowledge their ignorance and emit a bit of fear of making a mistake. My oncologist’s job is to worry about wandering cancer cells. All three of them do an outstanding job -- I am still here, after all — but they are not experts in the long-term care of the cancer patient.
At first I didn’t want to go to Survivorship Clinic. I feel a little like a faker being called a cancer survivor. Both because I still have plenty of cancer in my abdomen (it just hasn’t gone anywhere for two years) and because I am doing really well.
It turns out that people with cancer are considered survivors the day after we get our diagnosis. Whether we have survived one day, one year or 10 years, people use the word survivor to describe our status. I am not sure I agree with the use of the word this way and to be honest, I probably went to Survivorship Clinic to please my friend and because I thought the physical therapist might give me stretching exercises to do after I jog. Not because I identify as a survivor.
Over two hours, I met with a nutritionist, a physical therapist, a social worker and a nurse practitioner. The nurse practitioner had meticulously reviewed my chart, checked into all my prevention needs, and made recommendations with full knowledge of my cancer status.
“You need to get a mammogram,” she told me.
What woman hears this and thinks to herself, “Great news”?
A survivor.
Preventative health measures -- including mammograms, pap smears, good nutrition and regular exercise -- are important for people who are going to live for 10 years or more. For the same reason that women in their 80s don’t need these things -- something else is likely to kill them before a small breast or cervical lesion -- people with metastatic colon cancer don’t need them either.
Until they do.
Apparently I am doing well enough that I need to get back on that bandwagon of preventive care. So long, as-much-chocolate-cake-as-I-want-because-I-have-cancer. Hello, mammogram.
And having heard the rest of the recommendations for me from Survivorship Clinic -- balance exercises, hearing test, eating well and exercising -- I am a believer in the specialized clinic and maybe even calling myself a survivor.
A pediatric oncologist friend of mine, knowing she won’t get everyone to Survivorship Clinic, throws a survivorship picnic for her pediatric patients and their families every summer. Near the bouncy house, there are tables of information on eating well for cancer survivors. Next to the balloon stand there are places to sign up for hearing tests. There are trivia games and cooking lessons. And 400 people come every year. It’s not quite personalized follow up for a cancer survivor but it’s a start.
As more and more of us survive, primary care docs will become better versed in our care. Until that point, we need specialized follow up care that reminds us to exercise, eat our vegetables and yes, get mammograms.
Marjorie S. Rosenthal is a pediatrician at Yale and a 2015-'16 Public Voices Op-Ed fellow.