Advertisement
Health Coalition: We Can Reduce Costs Without State Regulation
Resume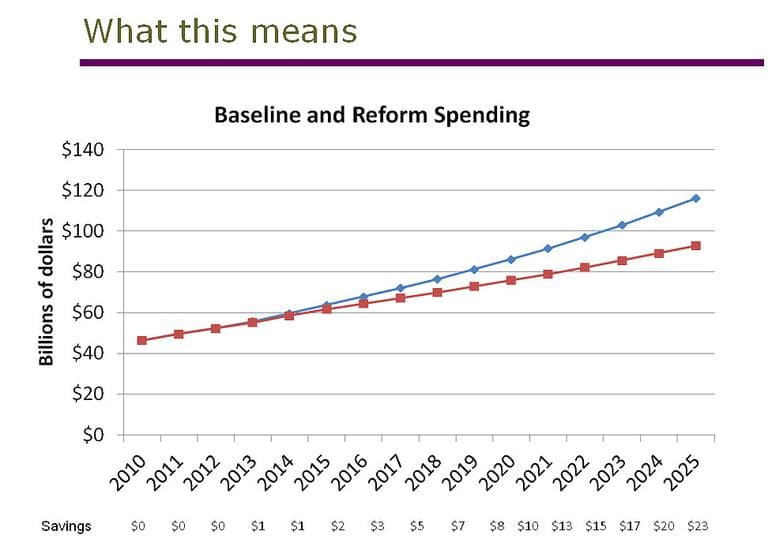
A coalition that includes health care industry leaders in Greater Boston and health economists has put together a draft plan for how to bring health care costs under control.
The message from the Eastern Massachusetts Healthcare Initiative to Gov. Deval Patrick and the Legislature is: we can reduce spending without more government regulation. More regulation, the group says, might make things worse than they are now.
WBUR's Martha Bebinger joined All Things Considered host Sacha Pfeiffer to detail the plan.
-- Here's the coalition's plan (on Scribd):
http://www.scribd.com/doc/71498512/Eastern-Massachusetts-Healthcare-Initiative-Payment-Reform-Recommendations
This program aired on November 3, 2011.
