Advertisement
Study: Can Teens Retrain Their Brains To Be Less Depressed?
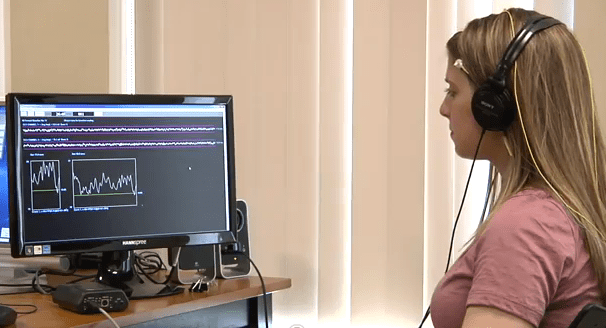
The half dozen electrodes were stuck to my forehead and scalp with cool gel. I leaned back in my chair and watched a white line representing some of my own brain waves spike up and down on the desktop computer screen.
“Hello there, brain of mine,” I thought.
When the white line rose nicely, meaning that I was headed toward a better mood, I was rewarded with pleasing xylophone-like music on my headphones. When the line fell, I heard nothing but silence, a signal that I was on the wrong track. It didn’t help to think of ice cream sundaes and glowing sunsets. And trying to will the line to go up did nothing. I just had to sit back and let my brain drive.
This curious technique, described as “a process of showing the brain to itself” in real-time, is called neurofeedback.
My small taste of it came courtesy of the system used in an experiment now under way in Cambridge and Providence to see whether teens can better fight depression by reshaping their brain activity. (The study’s Website is here.)
You may have heard of biofeedback, a decades-old method aimed at helping people train themselves to control their own blood pressure and other physiological functions. Neurofeedback is that for the brain, aimed at helping it learn to change itself, in an automatic response to reward or lack thereof.
Some clinics already offer neurofeedback sessions commercially for Attention Deficit Hyperactivity Disorder, and scattered studies have explored whether it might be helpful for other brain problems ranging from Post-Traumatic Stress Disorder to headaches.
Research on whether neurofeedback might be useful for mood disorders like depression is in its infancy, and the study under way in Cambridge and Providence is apparently the first to look at whether the method can help lift depression in teens. Initial studies have found positive results for depression in adults, but further, better-controlled research is needed.
Free, no drugs — but few takers
I’d have thought would-be subjects would be lining up for the teen depression study. Depression is endemic, especially in teens. Neurofeedback is non-invasive and drug-free, and not known to cause any adverse effects. The study offers a potential treatment that would normally cost more than $2,000 and probably not be covered by insurance. And it’s being run by academic psychologists from not-so-shabby institutions: Laurence Hirshberg of Brown, Fred Rothbaum of Tufts and Matthew Nock of Harvard.
But no.
The study’s staffers contacted CommonHealth because they were seeking publicity in hopes of finding the six or eight teens they need to sign up. Colleagues had warned Laurence Hirshberg that adolescents with depression are known as hard to enlist, he said. But still, he has been surprised at how uphill the recruitment has been.
Subjects sign up for a 20-session stint over 10 weeks. They rate their mood using a well-accepted questionnaire for detecting depression, and researchers watch for any change from an initial mood baseline.
Advertisement
How it works
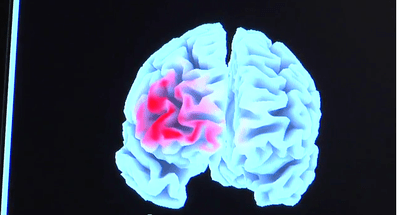
I asked Laurence how neurofeedback might lift mood, and he obliged me with a nicely simplified explanation of the study’s focus on the prefrontal cortex, the area of the brain that is just behind the forehead and considered the seat of rational thought.
The left side of the prefrontal cortext tends to be linked to more positive thinking and mood, he said, and the right side to more negative thinking and mood. So we want to train the brain to activate the left side more. The white line I watched on the screen reflected how active the “alpha” brain waves of my left side were compared to my right side. When the left was more active, the line went up and the music played.

In three studies done in non-depressed college students, Laurence said, brain training to activate the left prefrontal cortex more than the right did appear to improve mood. The subjects’ “cognitive patterns” started to change.
For example, he said, say you have a choice between two jobs, and you choose one. In healthy people with good moods, if you ask them six months later whether they made the right choice, they’ll tend to say yes — they’ll “organize their thoughts to fit the decision.” Depressive people will tend to to do the opposite, to say “Oh, I made the wrong decision again.”
The studies found that training to activate the left prefrontal cortex more appeared to help people “develop an opinion that supports their own judgment.” The data suggest that when the left prefrontal cortex is more active, he said, “the cognitive patterns associated with depression are less prevalent.”
Reality checks
This was sounding so promising that I thought I’d better get some reality checks. I spoke with Susan Parks-Cohen, a staff neuropsychologist at Harvard’s renowned McLean Hospital. Laurence had said that academia had tended to “look askance” at neurofeedback, but that as data accumulated and technology improved, that was changing. Was it really?
Susan confirmed both the “askance” period and the signs of change. For a long time, she said, it wasn’t clear how well neurofeedback worked, and how much of any observed changes might be merely placebo effects. But “it’s starting to be looked at in the field as a more reliable treatment option,” she said, “and one litmus test I see is that it’s started to be partially reimbursed by some insurance companies.”
They have even created a code so that it can be billed for, she said, and “in the field of mental health, it seems that insurance companies won’t cover something unless someone has convinced them that it works.”
Her sense, Susan said, is that neurofeedback remains on the “alternative” end of the treatment spectrum or as a supplemental treatment for depression. It is not replacing the traditional mainstays of medication and psychotherapy, but it might be considered among other alternatives such as EMDR — rapid-eye-movement therapy — or progressive muscle relaxation.
“Those kinds of treatment options I don’t feel are being commonly seen as first-line treatments,” she said, “but they are starting to gain some footing as alternative treatments.”
Susan has not referred her own patients for neurofeedback, she said, but has heard from respected colleagues that it helped some of their patients. And it has a particular emotional appeal, she said, because it could send patients a powerful message: “‘You have some ability to manage this.‘ It’s not all medicine, it’s not all ‘Therapist, cure me!’ It helps to give the patient some responsibility and some empowerment.
I also spoke with Signe Bray, a neuroscience researcher at the University of Calgary who has done neurofeedback experiments using a functional MRI machine rather than the EEG method used in the Cambridge study.
"The evidence that people can learn to modulate brain activation is there," she said. "Whether that effect is enough to overcome or improve clinical symptoms is still not really known. But it is something that people are interested in testing, and if you compare that kind of therapy to drug-based therapy, it’s probably preferable in many ways."
A third way
Laurence Hirshberg, who is a practicing clinical psychologist, said that he has seen neurofeedback help his patients, sometimes dramatically.
“I do all kinds of treatment and this is a really important form of treatment,” he said. “The fact that the science is really lagging behind the practice, and the fact that that’s not likely to change in the near future, doesn’t change the fact that it’s a useful intervention for people.”
He believes, he said, that there are now essentially three approaches to treatment: “One is psychopharmacology. One is psychotherapy. And the third is neurofeedback.”
I came away from my little taste of neurofeedback with a big idea of Laurence’s echoing in my mind. His three approaches to treatment could be put a bit more broadly: Drugs. Therapy. And what he calls “applied neuroscience.”
An example: Brain researchers have found reduced brain connectivity in autistic children. (See this week's Science Daily report on that here.) Neurofeedback researchers are taking that data and running with it, trying to increase the children’s brain connectivity and thereby improve their functioning, Laurence said.
New neuroscience findings on other disorders from PTSD to anxiety to learning disabilities could inspire similar efforts, he said: “There are a lot of possibilities that are just being looked at."
Below: the study's promotional video:
This program aired on July 29, 2011. The audio for this program is not available.

