Advertisement
Tragically Wrong: When Good Early Pregnancies Are Misdiagnosed As Bad
A beautiful, supremely talented young friend of our family recently fell victim to a terrible medical mistake. Newly married, she was having some pelvic pain and bleeding, and the doctor who saw her diagnosed a probable ectopic pregnancy — an embryo that develops outside the womb. Concerned that such pregnancies can turn life-threatening, the doctor prescribed the standard treatment: methotrexate, a drug used for chemotherapy and to help induce abortions.
When our friend returned to be checked a few days later, the imaging revealed that in fact, the pregnancy had not been ectopic; it was in place, in her uterus. But because she had taken the methotrexate, a known cause of birth defects, her pregnancy was doomed. She soon miscarried. What may have been a perfectly healthy pregnancy had been ended by well-meant medical treatment.
I assumed her horrifying case was an exceedingly rare medical fluke — until now. A paper just out in the prestigious New England Journal of Medicine shows that such misdiagnosed pregnancies are part of a pattern — a pattern that needs to be changed. "Considerable evidence suggests that mistakes such as these are far from rare," it says.
When I told our friend's story to the paper's lead author, Dr. Peter Doubilet, he responded that he knows of "dozens and dozens and dozens of similar cases that have come to lawsuits, and that's probably the tip of the iceberg." There is even a Facebook group, Misdiagnosed Ectopic, Given Methotrexate, run by a mother given methotrexate whose daughter was born with major birth defects.
The New England Journal of Medicine paper stems from a panel of international experts who resolved to change medical practice to stop such misdiagnoses. I spoke with Dr. Doubilet, who is senior vice chair of radiology at Brigham and Women's Hospital and a professor of radiology at Harvard Medical School. Our conversation, lightly edited:
Before we get into the nuts and bolts of the problem, what’s the upshot for women of child-bearing age? What’s your message to them?
When a woman gets pregnant, a number of serious complications can occur early in pregnancy, including miscarriage or ectopic pregnancy. When a doctor diagnoses these problems within the first two to three weeks after her missed period, it’s very traumatic to the patient and it’s critically important that the woman and the doctor are confident that the diagnosis is correct, because the steps that will be taken would harm a normal pregnancy if one is present.

It’s become apparent over the past two to three years that errors in diagnosis of miscarriage and ectopic pregnancy occur more frequently than they should, and that’s why we put together a multi-specialty panel of expert doctors from radiology, obstetrics-gynecology and emergency medicine to come up with new, more stringent guidelines for diagnosing these complications, taking into account the most recent research on the subject.
And just to simplify, when a woman in very early pregnancy has been told that it appears that she has an ectopic pregnancy or a failed pregnancy, it would very rarely be overly risky — and often be wise — to wait a couple of days and be sure of the diagnosis before acting?
Yes. That’s a very important message. In 2010, I, together with Dr. Carol Benson, wrote an editorial in The Journal of Ultrasound in Medicine entitled “First, do no harm to early pregnancies,” and that was the key message: Unless the doctor is sure that the woman has a miscarriage or an ectopic pregnancy, the doctor should err on the side of waiting, as long as the woman is stable and shows no signs of serious internal bleeding.
If the patient meets definite criteria for a miscarriage or ectopic pregnancy, there's no reason to wait, but if there’s any degree of uncertainty, the prudent thing is to wait.
Back in the 1980s and 1990s, doctors established rules for diagnosing miscarriage and ectopic pregnancy that were intended to provide definitive diagnoses of these conditions. However, research performed over the last few years has demonstrated that these rules, which are over 20 years old, are not foolproof. Responding to that research, our panel recommended making the criteria for diagnosing miscarriage and ectopic pregnancy more stringent.
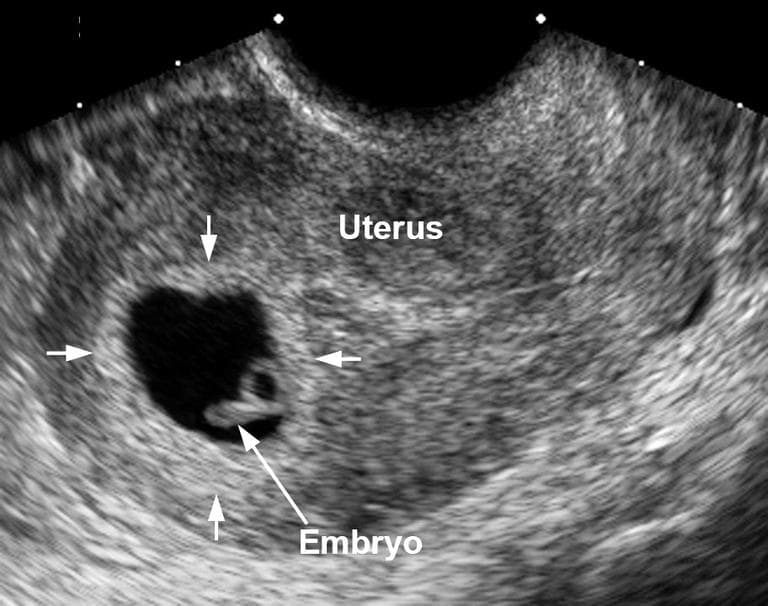
In other words, doctors tend to diagnose an ectopic pregnancy by saying: the patient's pregnancy hormone level suggests we should be able to see an embryo on ultrasound by now, but we don't, so it must be ectopic or a failed pregnancy. In other cases, they diagnose a miscarriage by saying: the embryo is large enough that we should be seeing a heartbeat, but we don't, so it must be a failed pregnancy. You'd be moving the hormone-level and ultrasound goalposts a bit to avoid the possibility of what you call “false positives,” meaning that you think the pregnancy is non-viable or ectopic when in fact it is normal?
That’s correct. In the paper, we talk about how in all of medicine we aim to be right all the time, but there's no way to fully achieve that goal. There are two kinds of errors in medicine: false positives and false negatives. In diagnosing ectopic pregnancy and miscarriage, we want to be absolutely sure not to make false positive diagnoses, especially if the patient is stable, so we set more stringent criteria for the exact purpose of avoiding false positive errors.
I’d imagine the counter-argument would be that ectopic pregnancies are known to be potentially life-threatening, and so doctors want to be able to err on the side of preventing life-threatening complications. How do you respond to that?
Great question. The answer is twofold: One is that with modern medical care, the risk of serious harm from waiting a couple of days in a woman who has an ectopic pregnancy but is stable is very low. And it’s especially low — we’re talking about women who have had a blood test and ultrasound — if the ultrasound doesn’t demonstrate any internal bleeding today. The risk of waiting a couple of days, even if she has an ectopic pregnancy, is very low.
And when you balance that very small risk against the terrible possibility of seriously damaging a normal intrauterine pregnancy, the balance is very clearly in favor of waiting if there’s any uncertainty. In order to address that important balance, we included on our panel not only radiologists like me, whose job it is to make the diagnoses, but also obstetrician-gynecologists and emergency medicine physicians who are the ones caring for the patient and making decisions about whether and how to treat the patient based on the diagnosis.
In the paper's financial disclosures, you mention testifying at trials on standards of ultrasound. Will anyone be able to accuse you of somehow playing to one side or the other of these cases with these new guidelines?
The medical malpractice work that I do is a very small fraction of what I do as a doctor, and I deal with cases as an expert for both the plaintiff and for the defense. Whichever side I take, I aim to tell them the truth as I see it.
I know there are no good numbers on this, but can you offer even a very rough ballpark estimate of how often you think these misdiagnosed pregnancies may occur?
I wish I could, but there are no national databases that keep track of medical errors.
Maybe just some back-of-the-envelope math? If there are maybe 6 million pregnancies a year in the U.S. and 2 percent are ectopic...
In terms of ectopic pregnancies, an all-too-common practice is to diagnose an ectopic pregnancy based on a blood test and an ultrasound at a single point in time. One of the key points that the panel made in the paper is that we cautioned against this approach when there is any uncertainty, and that’s because you’d often be wrong if you diagnose ectopic pregnancy based on a single blood test and ultrasound. One paper found that you'd be wrong as much as 40% of the time.
When you do a blood test and an ultrasound, there are three possibilities:
• The patient has a normal, intrauterine pregnancy
• The patient has a failed intrauterine pregnancy
• The patient has an ectopic pregnancy
The errors you really have to worry about, the really bad mistakes, are when you diagnose an ectopic pregnancy and it's actually a normal intrauterine pregnancy that would not have failed. And that's where we have no accurate data about how often this serious problem occurs, but we do know that it's far from rare.
Aside from the cases of women who have carried babies to term despite having been given methotrexate, how do we even usually know that this very serious error has occurred?
There are two problems that can occur as a result of administering methotrexate to a woman with an early intrauterine pregnancy: One is that the baby is born several months later with serious malformations. The other is a miscarriage.
Imagine the following situation, and this is what comes up all too frequently: A woman goes to the doctor in early pregnancy because she's having problems, usually bleeding or pain. The doctor does a blood test and ultrasound, diagnoses an ectopic pregnancy, gives methotrexate, and a few days later the woman has a miscarriage.
Sometimes the miscarriage is diagnosed when she passes tissue out, and the tissue is examined and proves to be a pregnancy that had been in the uterus. In other cases, the miscarriage is diagnosed on a follow-up ultrasound. You never know if the miscarriage would have happened even without methotrexate, but in all of those cases, we have to consider a distinct possibility, and even probability, that the methotrexate caused the miscarriage.
Just to clarify: If the pregnancy were actually ectopic, you wouldn't have the bleeding and passing of tissue of a typical miscarriage?
Actually, a patient with an ectopic who is treated with methotrexate may experience bleeding, but the material that passes out will not prove to be pregnancy tissue if it is examined under a miscroscope. The ectopic pregnancy itself shrivels up and goes away.
In all too many cases, a woman is diagnosed incorrectly as having an ectopic pregnancy, she gets methotrexate, comes back a few days later, has a repeat ultrasound, and now you see a failed intrauterine pregnancy. And the doctor says, 'Omigod, I gave methotrexate' — or the woman says, "Omigod, my doctor gave me methotrexate, now the ultrasound shows it's not ectopic, it's in the uterus.'
Why would they do the repeat ultrasound?
In many cases, the woman may have come in for bleeding and she has continued bleeding, so they do another ultrasound. In other cases, the follow-up ultrasound is done just to be sure that the methotrexate worked as intended.
Just to explain a bit more: In the 1980s and 1990s, doctors came up with that they called a discriminatory level of the pregnancy hormone HCG, which is measured in the pregnancy blood test. They said that if the HCG is above this discriminatory level but you don't see anything in the uterus on ultrasound, it couldn’t be a normal pregnancy. But recent research, including research we've done here at the Brigham as well as other places, has shown that the discriminatory level that was defined in the 1990s is not reliable for ruling out a normal pregnancy. That is one of the pieces of research that was considered by our panel, and one of our recommendations is not to treat patients based on the discriminatory level, because it's too prone to error.
So ultimately, is there anything sinister here? Was this overly defensive medicine being practiced with an eye to avoiding lawsuits? Or is this just the way of medical progress, that you create guidelines and then refine them?
There's absolutely nothing sinister. That one's easy. As medical science advances, we learn more, and come up with better methods for diagnosing and treating patients.
Can you offer a word of reassurance to all the women who’ve ever been told they had an ectopic or failed pregnancy and now are wondering whether that was correct?
Yes. Our goal here was to try to reduce errors to as close to zero as possible. We’re not suggesting that a high percentage of prior cases were diagnosed or treated erroneously.
In the majority of cases, ultrasound on its own or with blood tests is conclusive. The problems occur only in the relatively small percentage of cases where the ultrasound is not conclusive, and in those cases we need very strict diagnostic criteria before making diagnoses and initiating treatments that could damage an intrauterine pregnancy. Such cases are a relatively small percentage. But we want to get those errors down as close to zero as possible.
More broadly, as medicine advances, it’s a recipe for misery to go back and second-guess or fret over decisions that were made on the basis of accepted medical practice at the time they were made.
Readers, lingering questions? Please submit them in the comments below, and Dr. Doubilet is scheduled to speak on Radio Boston this Monday.
