Advertisement
Key Women's Heart Attack Symptoms Not So Different From Men's, AI Study Finds
If you die of natural causes, odds are it will be from heart disease, the top killer of Americans. So if you're having possible symptoms of a heart attack, get help fast.
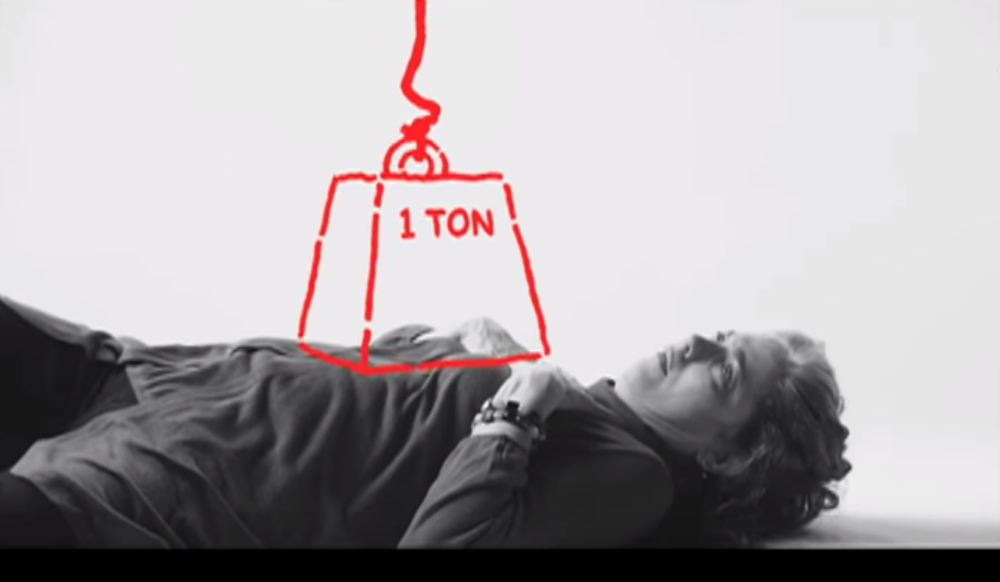
End of public service announcement, and now for some news on a big debate among heart specialists. The prevailing wisdom holds that women tend to experience heart attack symptoms differently from men. Men's symptoms tend to center on crushing chest pain, traditional thinking goes — that's long been known as "typical angina" — while women are more likely to have other or additional symptoms: fatigue, nausea, sweating, pain in the arm, shoulder or back -- that's known as "atypical angina."
But new Boston-based research used artificial intelligence to analyze how hundreds of patients described their symptoms in their own words, and it challenges that dogma.
The roots of the new research trace back a decade to a London street where Harvard Chan School of Public Health researcher Dr. Catherine Kreatsoulas saw a vivid picture on a double-decker bus of a man having a heart attack.
"He has this really squeezing sensation of like a belt that's made of his own skin that's squeezing him across the chest," she recalls. "And it said, 'Doubt kills. Call 999 if you're experiencing this type of pain.'"
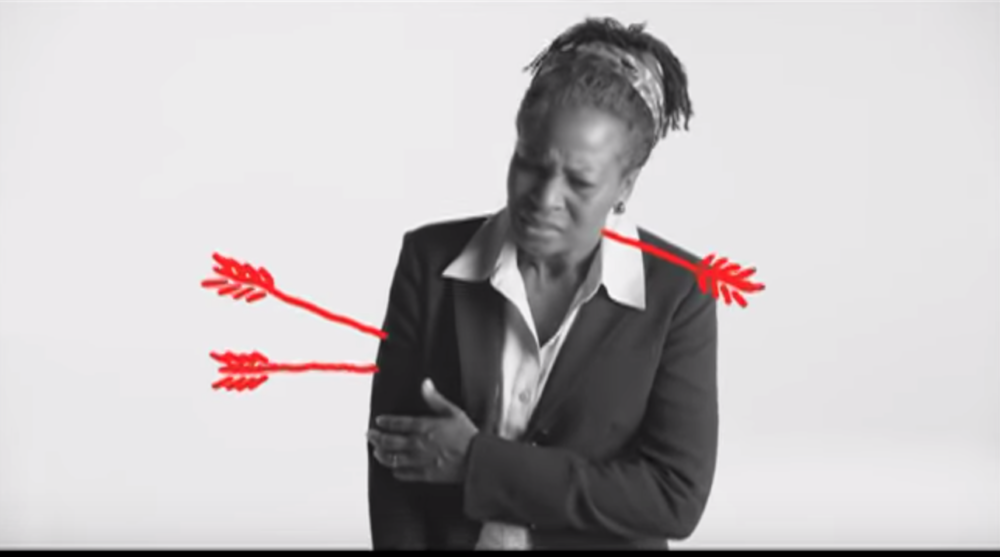
Kreatsoulas compared that image to a London hospital pamphlet that depicted a woman in a cardiac crisis holding her hands delicately crossed over her chest in a butterfly shape.
"And it looked like she was in a nice asana — a yoga pose," she says. "And I thought 'Wow! That's a really big difference. That's not how women present with heart disease when they're coming in for medical care.'"
"We see this in patients all the time, where they say 'Yeah, I was having crushing chest pain, but aren't women supposed to present differently?'"
Dr. Martha Gulati
In the years since, Kreatsoulas has explored that common perception — that men tend to have "typical angina" and women tend to have "atypical angina." Her latest study finds the medical reality is very different, says Dr. Deepak Bhatt, a leading cardiologist at Brigham and Women's Hospital, who also worked on the study.
It found, he says, "that widespread belief that men and women experience chest pain differently is probably not true. That is, of course there are differences between men and women, but in terms of chest pain, how they describe it is more similar than different."
The researchers audio-recorded interviews with more than 600 patients getting tests called angiograms for heart artery blockages, and used machine learning to analyze what they said and map symptoms onto their angiograms. (They use the new term "cardiolinguistics" for such study of heart disease-related language.)
Advertisement
They found that chest pain was the leading complaint in close to 90% of both women and men, Kreatsoulas says. "And the second leading symptom that is reported, both amongst men and women, is that they have trouble with their breathing, and they often complain of shortness of breath," she adds.
"Atypical" symptoms like dizziness and nausea were much less common, Kreatsoulas says, but both women and men reported them. Those rarer symptoms were not to be ignored, she says, "but the leading complaint is still chest pain."
The authors suggest that medicine abandon the terminology-- and the concept — of typical and atypical angina.
A 'Man's Disease'
That typical-atypical terminology has prompted much debate among heart specialists, says Dr. Martha Gulati, chief of cardiology at the University of Arizona and chair of the American College of Cardiology panel on chest pain guidelines. She was not connected with the study but saw it presented this month at a major cardiology conference.
The issue stems from 20th century studies of heart disease in which the patients as well as the doctors were overwhelmingly male.
"And so all our descriptors and terminology came from men, because somehow we didn't think of this as a disease that affected women commonly," Gulati says. "And now we know that's just not true. It's the number one killer of both men and women in the United States."
As the field has self-corrected and focused more attention on heart disease in women, Gulati says, findings about sex differences have sometimes been misinterpreted to mean that women don't get chest pain during heart attacks. Another misinterpretation: that "atypical" symptoms mean they are not heart-related.
"The word 'atypical' somehow got translated incorrectly in the medical community," she says. "Additionally, for patients or the public, when they are being given a public health message that somehow a woman's symptoms are different, then when they actually have very common symptoms, they think it's not a heart attack."
"We see this in patients all the time," she says, "Where they say 'Yeah, I was having crushing chest pain, but aren't women supposed to present differently?'"
Confusing Stories
The fundamental challenge is that patients who may be in a cardiac crisis tend to describe multiple symptoms, says Dr. Bhatt of Brigham and Women's.
"If you walk into an emergency room saying 'I'm having chest pain,' that gets everyone's attention and rightly so," he says. "But there's a whole constellation of symptoms that might be associated with blockages in heart arteries or heart attacks" or might not, such as arm or back pain, that confuse the picture.
The new study found that while the most prevalent symptom was chest pain, on average women reported nine symptoms and men reported seven.
Objective testing such as blood tests help, he says, and also the growing understanding that "it really is a matter of these symptoms occurring in conjunction with one another that is more predictive than in isolation."
Enter artificial intelligence, with its power to focus on many dimensions at once and paint a far more complex picture than traditional statistical methods or the binary terms "typical" and "atypical."
"Each patient is represented computationally as a unique fingerprint of symptoms where no two patients have the same fingerprint," says Dr. Karthik Dinakar, a research scientist at the MIT Media Lab who contributed the artificial intelligence piece of the study.
The methodology also allowed the patients' natural language to be analyzed, he says, avoiding the type of leading questions that could perpetuate misconceptions.
The method turned up distinct clusters of symptoms that could help sort through those confusing patient stories, the researchers say, and it could prove useful in other conditions — including a study already under way on Irritable Bowel Syndrome symptoms.
Listen To Your Heart
The AI study's findings jibe with other recent research, Dr. Gulati notes.
A big study called VIRGO found little difference in heart attack symptoms between younger men and younger women. And another study this month found that chest pain was the central symptom in more than 90% of both men and women.
In fact,"typical symptoms were more common in women than in men with myocardial infarction," it reports. It also found that women were more likely to report three or more symptoms than men.
Ultimately, Dr. Gulati says, the public message is two-fold: Women are more likely to report multiple symptoms, and "the majority of women present just like men."
Just to add one more nuance: It's not clear that "chest pain" is the best way to describe the central symptom, she says, "because often it really is a pressure-like symptom that people are reporting, or 'tightness.' As a physician, I'm often looking for other other cues," such as the patient's level of discomfort.
Dr. Bhatt from the Brigham offers a simple rule of thumb: If you're having symptoms like chest pain that are concerning, get checked. And if they're bad and escalating rapidly, call 911.
"People's internal sense of when something's wrong is actually good," he says. "If they listen. They often don't listen. But if they listen, it's pretty good."
This segment aired on September 17, 2019.
