Advertisement
Colonoscopy Culture Clash: Why Am I Getting One When Canada Says Not So Fast?
My last thought before drifting off was: What am I doing here?
As the nurse hooked up the IV for my "conscious sedation" — a pain-killing, amnesia-inducing, anxiety-easing cocktail of fentanyl and Versed — I had checked my phone one last time and up popped this headline: "New Canadian recommendation against colonoscopy for routine screening of colorectal cancer."
So why was I in the endoscopy suite on a recent Monday morning, my backside exposed in a hospital johnny?
Some background: I was supposed to get this routine colonoscopy when I turned 50 in 2014 but, like many people, I delayed — no family history and an emotionally tough year offered good excuses. When the year passed, I tried to procrastinate further, and asked my doctor about alternatives. "There are no real alternatives," she told me. "If there were another good option, I would choose that for myself but I will be having my colonoscopy this year as well."
As Dr. Ram Chuttani, chief of endoscopy at Beth Israel Deaconess Medical Center in Boston, put it: "Colonoscopy is still the gold standard."
So, of course, I made the appointment, ate the low-fiber diet, complied with the clear liquid fast the day before and suffered through the prep. (Except I was unable, at 4:30 in the morning, gagging, to finish the full 16 ounces of prep mixture.) Like countless other middle-aged Americans, sitting on the toilet en route to a pristine colon, I thought: There's got to be a better way.
Better In Canada?
Late last month, for the first time, Canadian medical professionals came out against colonoscopies for routine screening, saying that the evidence is lacking that this method is effective enough at preventing deaths from colon cancer.
"We recommend not using colonoscopy as a screening test for colorectal cancer," the new guidelines, published in the Canadian Medical Association Journal, say, in a summary.
So, if colonoscopy is the gold standard here but not recommended there, what's a patient to do? Maybe just acknowledge that different health systems, with different priorities and cost structures, end up promoting different flavors of medical care. What you should not do is nothing. If there's one thing pretty much everyone agrees on: colon cancer kills, but it's also largely preventable, so the best screening method is one that actually gets done.
The Canadian Task Force on Preventive Health Care, the group that wrote the new guidelines, cited two preferred colon cancer screening methods for low-risk, asymptomatic adults ages 50 to 74:
- Fecal occult blood testing (FOBT), in which stool samples are analyzed for hidden traces of blood, every two years
- Flexible sigmoidoscopy, which uses a scope to examine the lower part of the colon and rectum only, every 10 years (This procedure involves less prep than colonoscopy, no sedation, and in Canada it's done by either a nurse practitioner or primary care doc, with no specialist needed)
In America, the U.S. Preventive Services Task Force, an independent panel of medical experts that issues guidelines, recommends a range of colon cancer screening methods for low-risk adults 50 to 74.
Dr. Albert Siu, chair of the U.S. Preventive Services Task Force, told me in an email that the main point of the guidelines is simply to encourage screening.
“There are several effective ways to be screened for colorectal cancer, one of which is colonoscopy," he wrote. "The type of screening should be a personal choice, made in consultation with a doctor ... Colonoscopy, fecal occult blood tests, and flexible sigmoidoscopy are all screening options that effectively reduce the risk of dying from colorectal cancer. Our recommendation stresses the importance of getting screened."
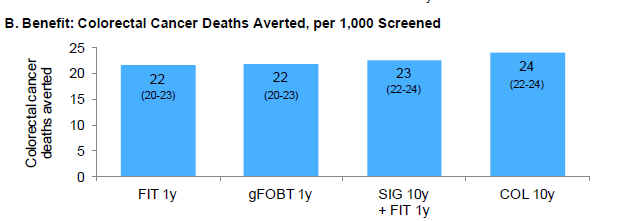
To that point, the task force website displays a graphic showing the number of colon cancer deaths averted per 1,000 screened. You might notice that the number of deaths averted by the various methods only differ from 22 to 23 to 24, with colonoscopy the highest, but not by much.
A Preventable Cancer
Nearly 50,000 Americans are expected to die of colon cancer this year. A high school classmate of mine recently died of the disease, shortly after being diagnosed. In the school newsletter, he conveyed his final thoughts through another friend: "Peter's final request was for everyone who is 50 or over or who has a family history to go get a colonoscopy ASAP. Please don't take chances with your health or your family's future."
Unlike some cancers, such as pancreatic or lung, most colon cancers will arise from pre-cancerous lesions called polyps, said Chuttani, the Beth Israel doctor. And if you remove them, you can often prevent the cancer.
"Having a pre-cancerous condition is, in a sense, the beauty of colon cancer screening," Chuttani said. "It's what makes it meaningful."
And, he adds, colonoscopy remains the best we have for picking up those early, smaller lesions; the various fecal blood tests are able to detect larger lesions that are much further along.
Regarding the Canadian guidelines, Chuttani said: "We ... were very surprised when they came out with the recommendations that they did; a lot is based on differences in their health system, they don't have wide availability of colonoscopy, there's a substantial waiting list."
Also, he said, the Canadians only looked at randomized controlled trials to come up with their guidelines, while the U.S. reviewed a broader range of studies, including observational studies. Notably, research published in the New England Journal of Medicine found that colonoscopy screening was associated with decreased incidence and deaths from colon cancer.
Chuttani said other screening methods, including virtual colonoscopy and alternative tests, simply aren't as effective as colonoscopy. Although he says colonoscopy is the “gold standard,” research has found a small "miss rate" for polyps.
"The final decision lies with the patient," he said. "We can only give them the best recommendation. There is good data ... that a single colonoscopy, done every 10 years, done well and done with a good prep, is the best way to prevent colon cancer. It's not completely fail-safe, there's a small but finite chance of missing the cancer, every test has its advantages and disadvantages."
He offers himself as Exhibit A. Chuttani got his colonoscopy three years late. He said he had no family history, and "was lazy." And lo, they found five polyps, including four not-so-small adenomas — some about a centimeter in diameter. When he went back three years later, he said, they found four more adenomas.
"That's nine polyps in the span of three years," he said. "If I was following the Canadian recommendation, I could possibly develop colon cancer in the next five to ten years."
And in fact, my very kind colonoscopy doctor ("Great prep!" she wrote on my discharge papers) did find two small polyps, which she removed.
Money, Risk And Evidence
Still hoping to avoid a colonoscopy? The Canadian recommendations did cause a little ripple of angst in the U.S. gastrointestinal community.
In a commentary on the American College of Gastroenterology blog, Dr. Dennis J. Ahnen, of the University of Colorado, writes that America is "a major outlier" when it comes to colon cancer screening, and the only country in which "colonoscopy is the dominant screening strategy." It's expensive and poses higher risks than other methods, he writes:
We should not be surprised when other countries make recommendations that differ from ours. I think that an important goal for the U.S. GI community is to make colonoscopy better and less variable in quality, to minimize colonoscopy risk and to make colonoscopy less expensive – particularly by not adding cost that hasn’t been shown to be of benefit (anesthesia as opposed to conscious sedation) and by not performing colonoscopy more frequently than guideline-recommended surveillance intervals.
Maria Bacchus, a general internist at the University of Calgary, Alberta, and chair of the Canadian guideline working group said in an interview that after analyzing high-quality, randomized, controlled trial data, the Canadians simply came up with different conclusions from their American colleagues.
"We found there was no direct evidence from high quality studies to show that screening with colonoscopy decreases mortality from colon cancers," she said.
Even among Canadian doctors, though, not everyone agrees. The Ontario Association of Gastroenterology issued a response to the new guidelines: “Colonoscopy is probably the best colon cancer screening test, it's just not proven yet.”
(Colonoscopy is recommended in Canada for high-risk patients such as those with a family history, a previous bout of colon cancer, a history of inflammatory bowel disease, or those with symptoms suggestive of colon cancer, Bacchus noted.)
Bacchus said that “screening with simpler tools” is just easier for patients and acknowledged long waits for colonoscopies in Canada and high costs as other considerations. If ongoing clinical trials show colonoscopy does save lives, the panel would certainly reconsider new evidence, she added.
A 'Nuclear Laxative'
As for me, the two very, very small polyps in my colon turned out be "benign" but potentially "precancerous" adenomas. I was told to come back for another colonoscopy in five years.
I asked Chuttani if, by then, I might have better options.
"I thought that by now we'd come up with something dramatically different and better, but for the next five to 10 years I don't see anything," he said.
But there may be a glimmer of hope. Dr. Joshua Korzenik, a gastroenterologist at Brigham & Women's Hospital in Boston, is trying to fix what is perhaps the most miserable aspects of the colonoscopy.
"One of the main reasons people don't do it," Korzenik said, "is fear of the prep. It's not the procedure itself so much, it's really the prep."
He cites Dave Barry, writing in The Miami Herald:
The instructions for MoviPrep, clearly written by somebody with a great sense of humor, state that after you drink it, ''a loose watery bowel movement may result.'' This is kind of like saying that after you jump off your roof, you may experience contact with the ground.
MoviPrep is a nuclear laxative. I don't want to be too graphic, here, but: Have you ever seen a space shuttle launch? This is pretty much the MoviPrep experience, with you as the shuttle. There are times when you wish the commode had a seat belt. You spend several hours pretty much confined to the bathroom, spurting violently. You eliminate everything. And then, when you figure you must be totally empty, you have to drink another liter of MoviPrep, at which point, as far as I can tell, your bowels travel into the future and start eliminating food that you have not even eaten yet.
On a flight home from a medical conference, Korzenik and a colleague decided that with only about 55 to 60 percent of people who should be screened for colon cancer getting it done, they had to act. "We should develop a better prep," he said.
After some at-home experiments followed by consulting with nutritionists and food experts, Colonary Concepts was born. The company is developing tasty bars and shakes for colonoscopy prep (with flavors like vanilla, strawberry banana, white chocolate and lemon) and working through the FDA approval process. Korzenik says the first products could be on the market within a few years.
Which leaves me hoping that when it comes time for my next colonoscopy, I'll be happily sipping a gag-free vanilla shake.
