Advertisement
Should You Take Aspirin? A New App Helps Your Doctor Advise You

Heart disease and stroke are leading killers, and I worry a lot about how to prevent them in my primary care patients.
One of the few proven interventions I can offer them is a daily low-dose aspirin. But aspirin has risks, and even after sifting through the data in a general way, I don’t always feel confident weighing them for a particular patient. Especially in the ever-shorter times I am allowed in a primary care visit.
One new solution is a decision tool called Aspirin Guide, released in June by Dr. Joann Manson and her colleague, Dr. Sammy Mora, both researchers at Brigham and Women’s Hospital. They created the app, available for the iPhone, along with developer Jeff Ames. It is free, and was not industry sponsored.
In an interview, Dr. Manson was understanding about my clinical indecision. “These are not back-of-the-envelope calculations,” she said.
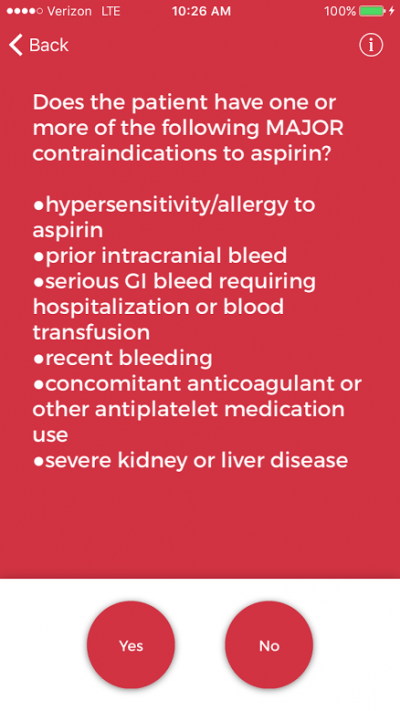
The app, which took me about five minutes to use, asks a series of questions about different risk factors for heart disease, such as blood pressure and cholesterol. It also asks about risk factors for bleeding, such as ulcers, as well as age and gender. Then it uses an algorithm to determine how helpful aspirin will be. The app also quantifies — for the first time in an easy-to-use format — an individual’s risk of a serious bleed.
Dr. Manson is hopeful that patients may use the app to “start a conversation” with their doctors, but does worry that patients may use the app to make their own decisions about starting or stopping aspirin. (Indeed, it has a disclaimer to that effect.) Instead, she says, the goal is that this kind of tool will lead to shared decision-making, which she called “the new frontier.”
Dr. Michael Hochman, director of the Gehr Family Center for Implementation Science, hopes that such decision tools can go even further and help patients drive the conversation with their providers.
“I would love to see it get to the point [that] it’s actually patients who are using these kind of support tools to decide if they would benefit from an aspirin, or a statin, or colon cancer screening," he says. "And not be pushed by someone’s bias either way.”
We doctors are not perfect, and certainly oversights and mistakes are made. As Dr. Mora pointed out in an op-ed about the app, for example, up to a quarter of patients who are unlikely to benefit from aspirin have been told to take it by their physician.
Apps like Aspirin Guide, in the hands of clinicians or patients, could push us further into rigorous, evidence-based medicine. Dr. Manson sees the potential applications as nearly limitless, and can imagine apps informing discussions on most new medications, when to start insulin for diabetes, and even in prescribing exercise regimens for patients.
In my last week as a primary care resident at Cambridge Hospital, I used this app for two patients. Both are engaged in their care, willing to take medications to reduce their risk of disease, and have important risk factors for heart disease.
Initially, I would not have prescribed aspirin for either one, because their risk was not high enough to make aspirin therapy clearly worth its own risk. After reviewing their data with Aspirin Guide, though, I am rethinking that decision. The app told me that aspirin was slightly more likely to benefit them than harm them.
I am hoping to have a conversation about this when they come back to the clinic. Maybe they'll even start it.
Regular CommonHealth contributor Dr. Elisabeth Poorman was a medical resident at Cambridge Health Alliance and plans to practice primary care. She’s on Twitter at @drpoorman.
Readers, if you try out the app, please let us know your experience.