Advertisement
Experimental Blood Test Detects Many Dangerous Cancers, Study Finds
An experimental blood test appears able to detect a wide range of cancers, according to research by the Dana-Farber Cancer Institute and others.
The study, published in the journal Annals of Oncology, found that when the blood test indicated a patient had cancer, it was almost always right.
"The test is designed to find cancers that shed DNA into the blood," says Geoff Oxnard, one of the lead researchers on the study. "And it seems like these are the more dangerous cancers, the higher-risk cancers and often the hard-to-find cancers." They include ovarian and pancreatic cancer.
The test didn't pick up all cancers, however — it missed about a third of them.
Dana-Farber is now launching a clinical trial of the test, Oxnard says, but testing is on hold now because of the coronavirus.
Interview Highlights
On the test
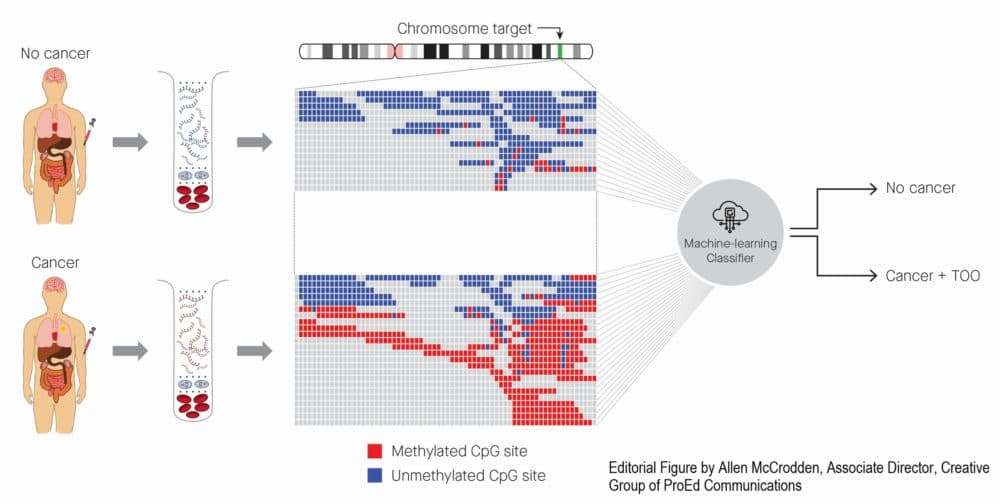
The test looks at free-floating DNA. This is a technology we use already in pregnant women to look for fetal abnormalities. And here, we're looking for cancer DNA. And what this blood test can do is find a wide range of cancers, advanced stage and early stage, a wide range of cancer types, and it can predict where the cancer came from with high accuracy. It's not perfect. It doesn't find all cancers. But it can find cancers with a low, low false positive rate.
In patients who don't have cancer, it only says that cancer is present less than 1% of the time. Moreover, when it finds a signal, the test can predict where the cancer came from so a doctor can go find it. And so it seems this is a noninvasive approach that should be developed further for broad-based cancer screening. And that's what we're doing.
The test is now being launched in clinical trials to actually give the blood test to patients at risk of cancer.
On current screening methods
The analysis focused on cancers that are often overlooked by current screening paradigms, dangerous cancers like pancreatic cancer and ovarian cancer. This is not instead of standard screening. So you would still get your mammograms and your colonoscopies as usual. But the hope is that a blood test used as a complement might be able to find some of the hard-to-find cancers that currently we are not able to screen for, like ovarian cancer and pancreatic cancer.
On when it might be ready for broad use
The good news is we're already using it now in select patients on a clinical trial in order to figure out and confirm that it's safe and effective and actually performs as expected. If these trials pan out, then we're certainly hopeful it'll be able to be offered more broadly to patients at risk of cancer in the near future. The timing depends upon how these trials pan out. What we've learned is that this test has the kind of performance that it deserves to be studied further. And that research is happening right now in big studies across the world.
On the study being funded by Grail, the company that makes the test
Dana-Farber is one of many sites participating in this study that was designed and run by Grail. What makes me impressed by the data is the size — this is, I think, the biggest effort that's ever been done of this type — the very rigorous analysis and the compelling results.
This study, CCGA, enrolled 15,000 individuals with cancer and without cancer. And in other studies, tens of thousands more patients are being analyzed. In the Pathfinder study that we've recently joined, we are giving results back to patients to figure out if actually they have an occult [undetected] cancer or not. Study enrollment is on hold now because of the coronavirus pandemic, but we're planning on getting it going again when possible, and hope to be able to make major progress on that later in the year.
On the methodology used
The first point to make is that cell-free DNA analysis is already used all over the place: It's used in pregnancy to look for fetal abnormalities; it's used in advanced cancer to help plan treatments. What we've done here is refine that approach to figure out exactly how to find cancer with a low false-positive rate.
We'd thought the best way to find cancer would be to look for mutations, because classically cancer is a disease of mutated DNA. But actually, we discovered that the blood is filled with mutations. These mutations are actually potentially benign mutations that are acquired as you age in your white blood cells. So looking for mutations is not going to be the solution.
Instead, through a lot of hard work, we figured out that it's methylation patterns that allow you to figure out where the cancer signal is without having false positives. Methylation is a way that the genes are turned on and turned off in the cell. We think this is how a skin cell knows that it's different than a heart cell or a lung cell. And if you use these methylation patterns, actually we discovered, quite surprisingly, that you can find a strong cancer signal in the blood without having the risk of false positives.
On speed
We are moving quickly here, and it really feels like we're making tremendous headway every month. And so I think that the potential for a really different paradigm for blood-based diagnostics exists in the next couple of years.