Advertisement
Inside the $11 million effort to help Massachusetts residents maintain health coverage
At the community health center in downtown Lowell, patient navigator Abbas Tanner made a phone call — one of dozens that he and his colleagues would make that day.
On the line was a 29-year-old woman from Leominster who needed help renewing her insurance from MassHealth, the state Medicaid program. Tanner asked a series of questions about her family, her income and her immigration status, typing her answers on his laptop.
"Has any information changed in regards to your tax filing status?" Tanner asked the woman. An interpreter, Maria Cruz, translated into Portuguese. After about 15 minutes, they renewed the patient's insurance under MassHealth.

This work of guiding people through the sometimes tedious task of obtaining health coverage is critical right now. It’s part of a sweeping effort across Massachusetts to help low-income families and individuals maintain access to health care during a turbulent time for MassHealth.
During the COVID health emergency, federal rules allowed Medicaid recipients in Massachusetts and other states to keep their benefits indefinitely, even if their income increased. But the grace period has ended. Now, people have to prove they qualify.
If for some reason they don’t receive their renewal notice, or don’t respond fast enough, they could lose health coverage altogether.
The burden is especially high for immigrants and communities of color who don’t speak English, or who lack easy access to technology.
"The patients and community members that tend to fall through the cracks are those that are most vulnerable," said Brenda Rodriguez, chief strategy and finance officer at Lowell Community Health Center. "They may not have a computer or working cell phone to follow through and fill out a form online, or they may have other barriers."
State officials are spending at least $11 million on a campaign to reach the 1 in 3 state residents who rely on MassHealth.
Advertisement
The stakes are high. Individuals who lose their insurance may be less likely to seek health care when they need it, or they could face big bills for care.
And there are broader implications. Massachusetts’ landmark 2006 health care law was a blueprint for the Affordable Care Act, and more than 97% of Massachusetts residents are insured. A decline in this number would be an embarrassment for a state that has developed a reputation for protecting access to health care.
"Universal coverage is our north star," said Mike Levine, assistant secretary for MassHealth.
MassHealth covers 2.4 million people. Levine said state officials hope to renew up to half of them automatically, using income data from public programs. They are trailing behind that goal but are working to reach it, Levine said.

The process of determining who is eligible for MassHealth launched in April and is expected to take a year. State officials are mailing tens of thousands of renewal notices in blue envelopes every month. Members have at least 45 days to respond.
But there are fears that people might not receive this important mail from MassHealth because they changed addresses. Or they may get the letter and not understand they need to respond.
The health policy nonprofit KFF estimates that between 8 million and 24 million people across the country will lose Medicaid coverage during this verification process — many of whom are eligible for benefits but get kicked off coverage because they don’t respond to renewal notices.
Already, data from states that have moved more quickly to trim their Medicaid enrollment shows that more than 70% are losing coverage for procedural reasons, such as failure to return forms, according to KFF.
Levine said this early data from other states underscores the need for outreach and education, so that people don’t lose coverage inadvertently.
"We are not going to stop trying to get that number to be as low as possible," he said.
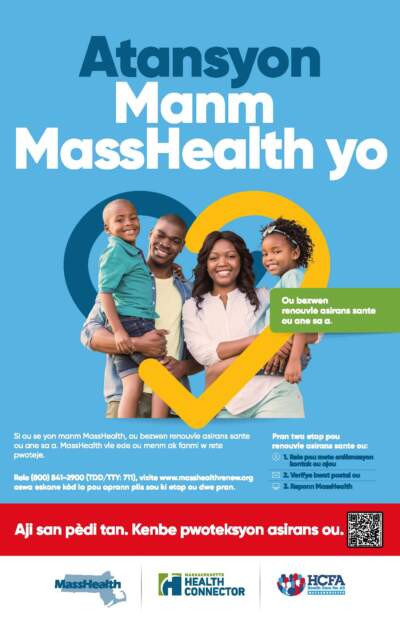
The state campaign to reach MassHealth members ranges from community events and TV ads to calls and text messages.
Information is available in nine languages: English, Spanish, Portuguese, Arabic, Haitian Creole, Cape Verdean Creole, Khmer, Chinese and Vietnamese.

Outreach workers are going door to door in Chelsea, Brockton, Framingham and a dozen other communities with big numbers of residents on MassHealth. They knocked on more than 260,000 doors and talked to 55,000 people in just two months.
"This is a massive undertaking," said Maria Gonzalez, who helped launch the outreach campaign at Health Care For All, a consumer advocacy group hired to work with the state.
If MassHealth members don't take action to renew, "there's a possibility that they may lose coverage — and that's what nobody wants," Gonzalez said.
Enrollment specialists, including those at Lowell Community Health Center, are working across the state to help people renew their MassHealth insurance, or move to other plans.
People who become ineligible for MassHealth may qualify for subsidized plans on the state insurance exchange, called the Health Connector — and about 16,000 have already done so. (Some Connector plans have premiums of just a few dollars a month.) Other people leaving MassHealth may be able to get health coverage through their employers.
Massachusetts is doing more than other states to help people maintain coverage. But advocates still worry it may not be enough.
"It looks like a mess to me," said Heloisa Galvão, executive director of the Brighton-based Brazilian Women’s Group, which works with Brazilian immigrants.
She said it’s cumbersome for people who don’t speak English to get information when they call MassHealth.
"It has to be done in a humane way," Galvão said. "If you're new here, and if you don't know how it works, and if you don't speak the language, it is scary, scary, scary."
State officials have set up a dashboard to track changes in MassHealth enrollment, though it’s too early to know how many people are losing coverage for failing to return forms, or other procedural reasons. At a recent public meeting, state health secretary Kate Walsh was bracing for a rough summer.
"People are going to show up for their kid’s school physical and hear they’re not enrolled," Walsh said. "That’s what we’re trying to avoid — but it definitely is going to be hand-to-hand combat."
This segment aired on July 5, 2023.
