Advertisement
A Dying Physician And The Meaning Of Care

Doctors die, just like the rest of us. But they do not die like the rest of us.
Ken Murray, M.D., explained this curious aspect of mortality in his widely circulated 2011 essay, “How Doctors Die." “What’s unusual about them,” wrote Murray, a professor of family medicine at the University of Southern California, “is not how much treatment they get compared to most Americans, but how little.”
In the early days of 2014, Kate Granger is living this truth. Like Murray, Granger is a doctor. Like Murray, Granger’s approach to her own mortality is influenced by her knowledge of medicine.
Diagnosed with an incurable cancer, Granger knows she will die quite soon. This knowledge, it seems, has reminded her how to live.
But Granger’s sense of her own mortality is different in this way: Diagnosed with an incurable cancer, Granger knows she will die quite soon. This knowledge, it seems, has reminded her how to live. She has traveled, renewed her marriage vows, made regular time for family, and continued to see patients. The things that matter most in her life, she is making time for.
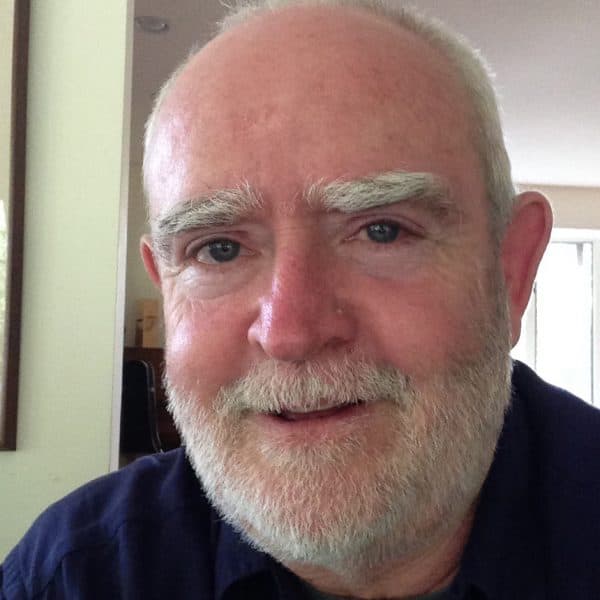
Granger, who is in her early 30s, specializes in elder and palliative care in England. Her deep and profound love of the elderly began in childhood tagging along with her mother, who ran a volunteer day center for elderly with mental health issues. “I loved chatting to the old folk there and learning about their lives,” Granger told me via email from Wakefield, England.
That she will not become elderly herself is tragic. That she is not wasting a moment of her time remaining is inspiring. That she is so generous with this time is breathtaking. She has written two books about her experience, and is working on a third. And such is her commitment to the doctor-patient relationship, and to public engagement in medicine, that she agreed to an email exchange with me.
Twitter led me to Dr. Granger. It was 2012, and I was discovering what’s known as the Liverpool Care Pathway for the Dying Patient, a remarkable set of hospice-inspired guidelines that died a horrible death amid a “death panel” type uproar in the United Kingdom. I began following her blog and her tweets.
Patients are first & foremost people. We have anxieties, opinions and ideas about our healthcare. Involve US in our care.— Kate Granger (@GrangerKate) January 16, 2014
The LCP caught my attention at a time when I was absorbed by the strange concept of “medical futility,” which is essentially a place on the timeline of patient care where one party determines that treatments no longer serve a therapeutic or curative purpose. It can be the patient who decides this but more commonly it is the doctor. Granger is both.
As a doctor, Granger knew the cold truth of futility, even before attempts to cure or slow the advance of her own terminal cancer. Her blog entry "Dear Chemo" movingly tells of her acceptance of both diagnosis and prognosis, and decision to forego another go-round of chemo.
Granger’s blog usually is devoted her own story, in her own words, but recently she shared a poet’s tribute to her: “But to inspire means to breathe in/and you inhale your life to the full,/determined to live for the moment/ to avoid the flat or the dull.”

Along with elder and palliative care, Granger is a specialist in communication. I’d begun to think some doctors are simply not cut out to be good communicators, and I’m encouraged that Granger says I’m wrong. Communication can be learned, she says; it just takes effort. Her own illness has made her an even better communicator. From our email exchange:
“I am incredibly protective of patients in my care who are dying. I invest a lot more emotional energy in conversations with them and their families than I did before I was ill. I am very keen to determine their wishes and will work very hard to get them out of hospital safely if that is what they want. This has meant staying late on many occasions.
“I am much more aware of my own body language now; I will always kneel beside the bed or sit down so I am on the same level as my patient and I use touch much more during difficult discussions. I don’t usually tell patients or relatives that I’m ill, but I think it just makes me able to understand on a deeper level what they are feeling and makes it easier to engage in conversations about difficult stuff such as fears for the future.”
As to her own fears, I don’t doubt that she engages them in the right way, at the right time, with the right set of ears. But in the same email in which she matter-of-factly told me, “I’m going to die in the next few months,” she began with “Hope you had a wonderful Christmas. Mine was just perfect.”
I believe she meant every word.
Related:
- Also by Paul McLean: Medical Ethics And The Blurred Boundaries Of ‘Do No Harm’
- Death In 140 Characters