Advertisement
Commentary
'My Patients Are Sicker Than Ever': The Pandemic's Collateral Damage

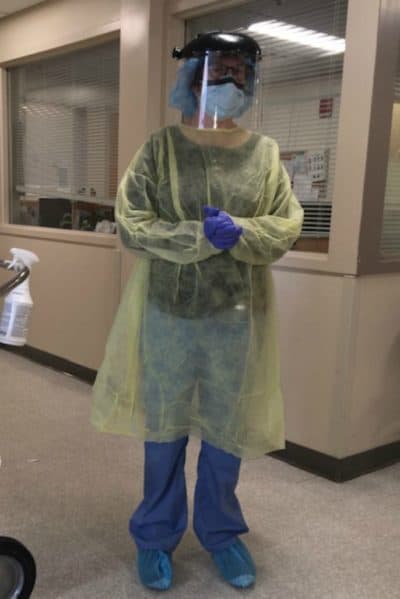
In some ways, my work at an urban community health center these days is less taxing than it was last spring, during the height -- so far — of the pandemic. I wear my own clothes again. No more long shifts in a COVID-19 testing tent, in full PPE. I'm working pre-pandemic hours. Best of all, I see my primary care patients in person again. (I also continue to do some telemedicine.)
When I see patients, I still wear a KN-95 mask and face shield, which make dents in my face and hair, fog up, cause skin break-outs and make certain medical procedures difficult. Try looking in an ear canal through a scratched and smudged face shield. I do not hug my patients despite desperately wishing I could. Sometimes a hug says what all the words in the world cannot.
Still, I find my heart breaking at work daily. More of my patients than ever before are getting sicker. In the past month or two, more of my patients have been admitted to the hospital and I have sent more patients to the ER for evaluation (and eventual hospital admission) than I can ever recall. In one week, three of my patients had strokes. Several other patients were admitted with heart attacks or heart failure. Others had severe electrolyte abnormalities or anemia, requiring transfusion and intervention.
My colleagues share my experience. Why are so many patients falling ill? Some lost insurance during the pandemic due to employment changes, which meant they couldn't afford their medication, which then caused their illnesses to flare. Others were isolated and alone, without anyone to monitor them, their symptoms and their medications. Many patients could not afford basic food; certainly the cost of fresh fruits and vegetables was prohibitive. This created a perfect storm of poor nutrition, physical inactivity, isolation and poor access to medications, resulting in poor health.
This pressure cooker of the COVID-19 surge aftermath, combined with the uncertainty in our country's government ... has everyone on edge.
Patients who were scheduled to see specialists, either for chronic disease follow-up or work-up of new symptoms, during the spring and early summer had their care postponed due to the COVID surge. Surgeries were delayed. Testing was pushed out. In some cases patients had been waiting months for this specialty care, and now pandemic circumstances forced them to wait even longer. Most specialist management of complex diseases was effectively put on hold, leaving time for those diseases to worsen.
Some patients are still afraid to come to the office. One of my patients had a panic attack upon entering the building and needed to leave immediately. We do what we can using telemedicine. We distribute home blood pressure cuffs and glucose monitors. Still, sometimes we need to see patients in person.
Patients' mental health is suffering. Parents are forced to choose between working and making money versus supervising remote schooling of their children. Children with special needs who thrive in a structured environment are suffering and acting out, and their parents are stressed and at a loss for what to do. Adults caring for elderly parents have to make similarly difficult choices about how to best care for their elders. Adult daycare is less available, so the burden of care falls on the adult children. Many of these adult children are balancing care for their own school-aged children, while trying to hold down a job.
Advertisement
Other patients are isolated, confined to small apartments or rooms in a boarding house. Patients are anxious and depressed, suffering panic attacks and insomnia. Fortunately, we have wonderful therapists and community health workers who meet with patients remotely. Many patients are more likely to accept counseling and assistance when they can talk from home, by phone.
Many of my patients are essential workers. Some worked extra hours to cover staffing gaps. Others did not have access to adequate PPE. These essential workers left their children, elderly parents and other family members at home for long stretches of time, and they continue to do so. This all takes a toll.
This pressure cooker of the COVID-19 surge aftermath, combined with the uncertainty in our country's government and the fear about its current leadership has everyone on edge. While the election results provide hope, the time when we can freely circulate in society without fear of contracting COVID-19 seems so far away. People feel a loss of control in all aspects of their lives, and sometimes they take it out on our health center staff. Any misunderstandings about promises regarding prescriptions, letters or appointments can lead to tempers flaring, acting out and unsettling behavior which has a ripple effect on everyone.
We are short-staffed, and everyone is working to their max. Patients desperately want to speak with their providers, but providers have a limited amount of time and emotional resources. There is the incessant nagging feeling that there is more to do, tasks are neglected, work could always be done better. Most importantly, we need to acknowledge that racial, ethnic and class disparities are real, front and center, causing great suffering in our community, and need to be addressed.
I fear for the future. I am worried about the upswing of COVID cases, particularly during the winter months when influenza infections rise. I am concerned for the impact of the economic and social fallout of the pandemic on people already living in poverty, who rely on an ever-weakening safety net.
I am heartened by the phenomenal work my colleagues do each day. Love and dedication are in steady supply. Our patients inspire us. They possess incredible inner strength and resilience, continue to express deep gratitude and concern for our safety, put one foot in front of the other each and every day, and against so many odds, continue to have faith that this world can improve.
