Advertisement
Brain Scans To Help Determine Treatment For Depression?
A diagnosis of depression is usually followed by months of uncertainty and experimentation. Should I try talk therapy first? Are medications the answer? If so which ones, and how long will I have to wait to know if they're working?
But a new government-funded study suggests there may soon be a way to decide by looking at brain scans.
If the part of the brain called the insula is overactive, the patient should be prescribed medication, the study indicates; if the insula is underactive, than cognitive behavioral therapy, a type of talk therapy, may be better.
This power to predict, if confirmed by other research, will help avoid months of trial and error treatment, and – though brain scans are costly – might save money in the end, by getting the patient effective care much faster, said Diego Pizzagalli, director of the Neuroimaging Center and the Center for Depression, Anxiety and Stress Research at McLean Hospital. He was not involved in the study.
Published in today's issue of JAMA Psychiatry, the study also reinforces the idea that depression is not one condition, as it's currently defined in the "bible" of psychiatry – the newly published edition of the Diagnostic and Statistical Manual.
Instead, Pizzagalli said, it's a wide-ranging set of symptoms that experts have decided should be called depression. Psychiatrists are currently debating whether such symptoms – or the underlying biology – should be used to define psychiatric conditions.
"What we are learning through our work is that basically the diagnosis of depression does not map one to one to biology," said Pizzagalli, also an associate professor of psychiatry at Harvard Medical School. "Using neuroimaging we can differentiate between subgroups of patients in important ways."
Pizzagalli said he is optimistic that imaging, along with hormones in the blood that indicate stress or markers that show inflammation, will eventually allow psychiatrists to do a much better job of diagnosing and treating people with mental health challenges. "We are getting closer to the day when we will be able to guide treatment selection using more objective markers," the neuroscientist said.
The new study, led by Dr. Helen Mayberg at Emory University in Atlanta, looked at PET scans from 63 depressed, untreated patients, and then divided them randomly into two groups, with half receiving cognitive behavioral therapy and half the anti-depressant escitalopram (brand name Lexapro) for 12 weeks. Activity in the insula, which is involved in emotional states and perceiving bodily sensations, predicted which treatment they would fare better on, the study showed.
From the press release:
“For the treatment of mental disorders, brain imaging remains primarily a research tool, yet these results demonstrate how it may be on the cusp of aiding in clinical decision-making,” said NIMH Director Thomas R. Insel, M.D.
Currently, determining whether a particular patient with depression would best respond to psychotherapy or medication is based on trial and error. In the absence of any objective guidance that could predict improvement, clinicians typically try a treatment that they, or the patient, prefer for a month or two to see if it works. Consequently, only about 40 percent of patients achieve remission following initial treatment. This is costly in terms of human suffering as well as health care spending.
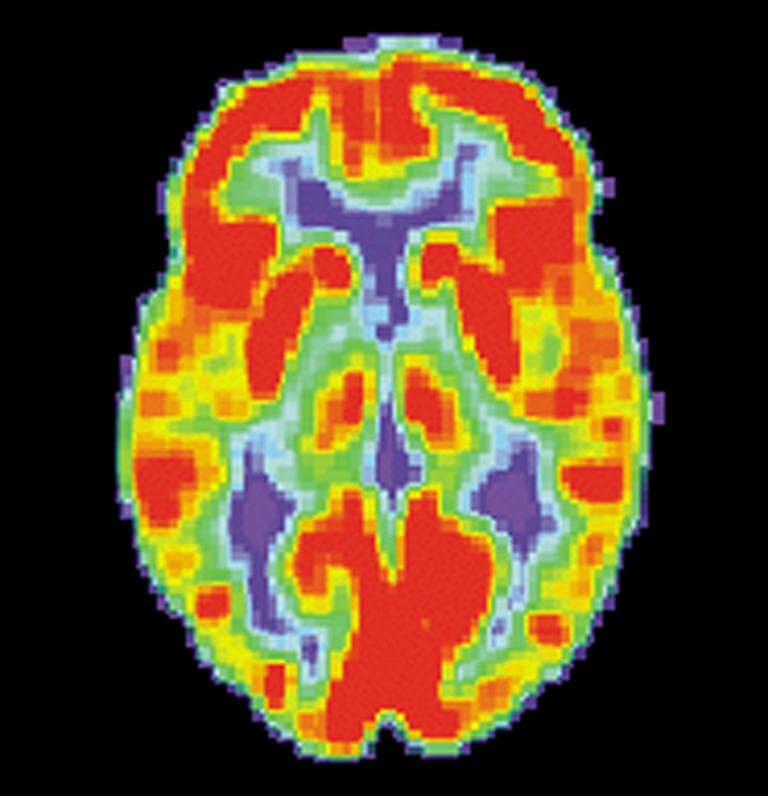
Mayberg’s team hoped to identify a biomarker that could predict which type of treatment a patient would benefit from based on the state of his or her brain. Using a positron emission tomography (PET) scanner, they imaged pre-treatment resting brain activity in 63 depressed patients. PET pinpoints what parts of the brain are active at any given moment by tracing the destinations of a radioactively-tagged form of glucose, the sugar that fuels its metabolism.
They compared brain circuit activity of patients who achieved remission following treatment with those who did not improve.Activity in one specific brain area emerged as a pivotal predictor of outcomes from two standard forms of depression treatment: cognitive behavior therapy (CBT) or escitalopram, a serotonin specific reuptake inhibitor (SSRI) antidepressant. If a patient’s pre-treatment resting brain activity was low in the front part of an area called the insula, on the right side of the brain, it signaled a significantly higher likelihood of remission with CBT and a poor response to escitalopram. Conversely, hyperactivity in the insula predicted remission with escitalopram and a poor response to CBT.
Among several sites of brain activity related to outcome, activity in the anterior insula best predicted response and non-response to both treatments. The anterior insula is known to be important in regulating emotional states, self-awareness, decision-making and other thinking tasks. Changes in insula activity have been observed in studies of various depression treatments, including medication, mindfulness training, vagal nerve stimulation and deep brain stimulation.
So when will this be coming to a clinic near you? Unclear. "Of course studies will be needed to replicate this finding," Pizzagalli says.
This program aired on June 12, 2013. The audio for this program is not available.