Advertisement
AG Healey Reaches $1 Million Settlement With 7 Companies To Increase Behavioral Health Access
Seven health care companies have agreed to take steps to improve access to behavioral health care in Massachusetts.
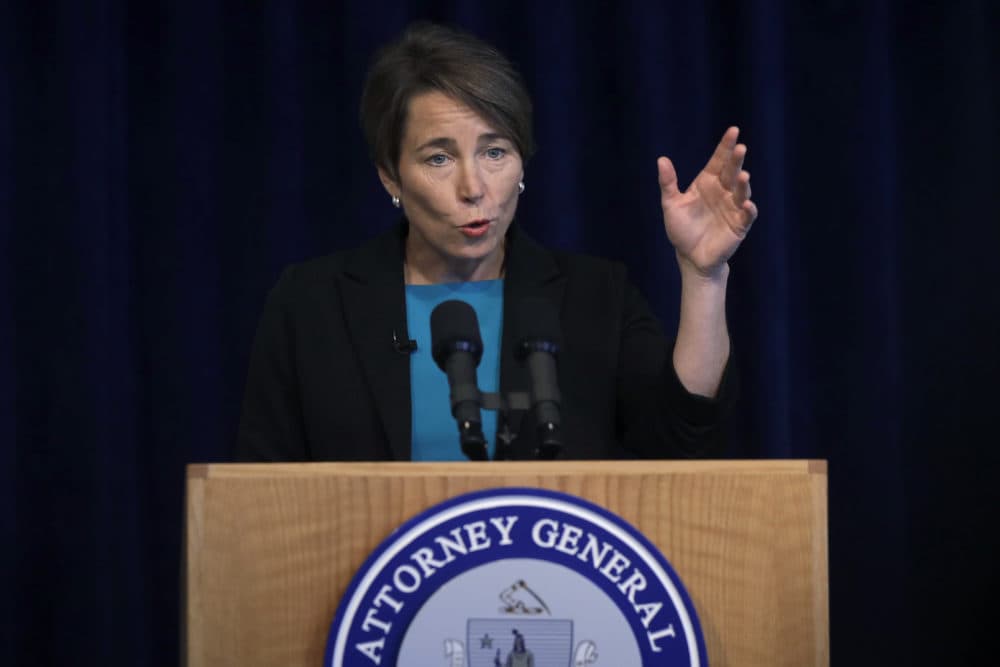
State Attorney General Maura Healey announced Thursday that her office reached settlement agreements with all seven companies — including five health insurers — to change their practices and pay a total of $1 million. She said the changes should affect about one million Massachusetts residents.
Healey's office said the charges involve the companies limiting access to mental health and substance use treatment in several ways.
"People shouldn't have to jump through hoops in order to get coverage for mental health care," Healey said at a press conference Thursday. "They shouldn't have to be forced to go out of network, or pay out of pocket because our system unfortunately has been designed in a way — or at least has resulted in a way — that there's this disparate treatment in the way we treat behavioral health and the way we treat physical health."
The companies are:
- Harvard Pilgrim Health Care and United Behavioral Health doing business as Optum
- Fallon Community Health Plan and Beacon Health Strategies
- Allways Health Partners
- Blue Cross Blue Shield of Massachusetts
- Tufts Health Plan
Three of the companies — Harvard Pilgrim Health Care, Fallon Community Health Plan and AllWays Health Partners — earlier resolved claims that they violated the federal Mental Health Parity and Addiction Equity Act by paying less for behavioral health care than physical health care. They agreed to change how they establish reimbursement rates. They also agreed to limit some prior authorizations for behavioral health care.
Healey's office also alleged that the three companies imposed unlawful barriers, including prior authorization requirements, for behavioral health services that were not required for comparable physical health services. The companies agreed to change some of those requirements.
"It's not lost on me that the state's first parity law will be 20 years old this May," said the state's Secretary of Health and Human Services Mary Lou Sudders. "And perhaps we can finally say we will have achieved parity in Massachusetts."
Advertisement
Blue Cross Blue Shield of Massachusetts and Tufts Health Plan were cited for not properly managing behavioral health provider directories. Healey cited a 2018 federal government report which found nearly half of provider directories for Medicare Advantage plans displayed missing or inaccurate information. All seven companies agreed to improve directory information and make changes so patients can more easily identify behavioral health providers.
A statement from Blue Cross Blue Shield of Massachusetts said the insurer agrees that provider directory accuracy is important, and it has supported legislation to improve those systems. It also said it is committed to providing quality treatment to its members and has taken several steps to help members better access treatment.
"We are recognized as a local and national leader in supporting members with substance use disorder (SUD)," the BCBS statement said. "We've taken unprecedented steps to ensure that our members get the care they need, when they need it, by removing barriers to access and matching those in need of SUD services with licensed, credentialed providers."
The Massachusetts Association of Health Plans said it welcomes guidance on how best to follow federal parity laws.
"To ensure a clear and consistent application of the federal law in Massachusetts, it is imperative that the Attorney General and state agencies work together to establish a uniform interpretation of the federal mental health parity law and issue state guidance so that Massachusetts consumers, employers, providers and health plans can understand their rights and responsibilities under the law free of competing interpretations," said a statement from Lora Pellegrini, president and CEO of the Massachusetts Association of Health Plans.
All seven companies will each pay toward the $1 million settlement. The AG's office said the money will go to a fund that will be used by her office to promote initiatives designed to prevent or treat substance use disorders, increase access to behavioral health care services, or otherwise assist Massachusetts behavioral health care patients.
This article was originally published on February 27, 2020.
