Advertisement
'It's Taking Up My Entire Day': Hospitals Prepare For A Possible Wave Of Critical Coronavirus Patients
Resume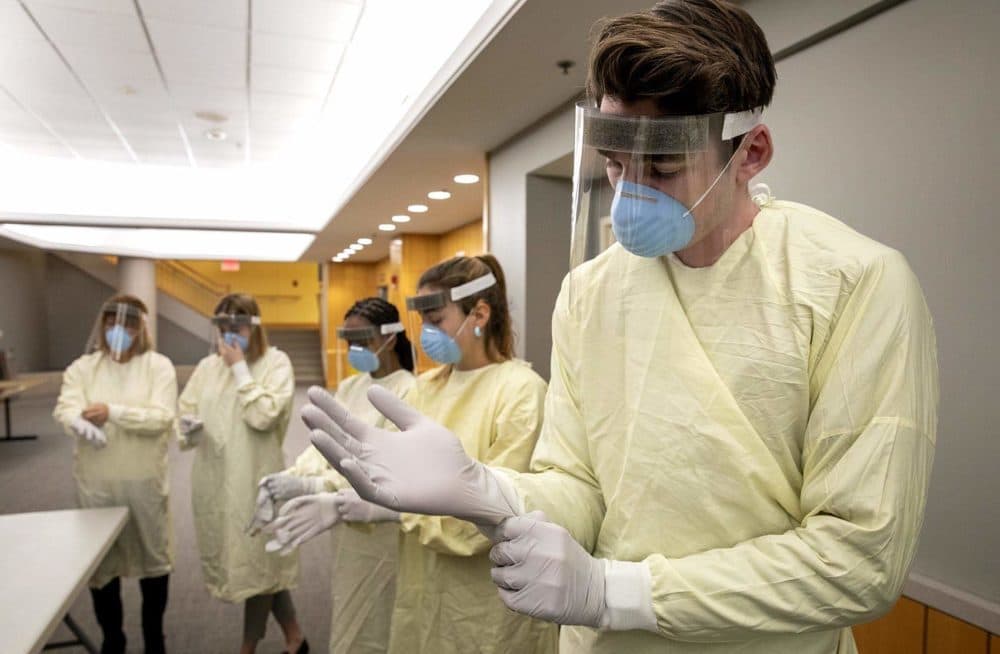
Tufts Medical Center doesn’t look “very different yet,” says Dr. Shira Doron, the hospital’s epidemiologist. “There’s a relatively high volume of patients in the clinics, especially the primary care clinic. It’s not a ridiculously high volume at this point.”
But it might soon be.
Doron, along with other doctors and hospital managers all over the country, is preparing for the possibility her workplace might see a sudden surge of patients with COVID-19, the illness caused by the coronavirus. Those patients may need intensive care.
As of Sunday, Massachusetts had reported 164 positive tests for the coronavirus, and officials announced that the data suggest community spread in seven of the state's 14 counties. Gov. Baker introduced aggressive measures to try and stem the spread of the virus, but the number of reported cases is expected to increase even further as testing ramps up.
While public health officials have emphasized that the virus causes only a flu-like illness for most people, it can require hospitalization, especially for the elderly and people with underlying health problems.
To get ready, hospitals have activated what they call “incident command centers” – systems designed to manage emergencies.
And the incident command center at Tufts has become a flurry of activity, Doron says.
“Key hospital leaders all sitting around a table on their computer and phones and discussing strategy,” she says. “A lot of white boards and pieces of paper taped to the wall, things like that.”
One of the key discussions is how many extra intensive care beds might be needed in the coming weeks and where hospitals might put them, Doron says. Nobody knows just how many patients will be in critical condition as the coronavirus spreads, but doctors and researchers are looking to the experiences of other countries to make an estimate.
The first region hit by the coronavirus epidemic, which has now been declared a pandemic by the World Health organization, was the city of Wuhan, China. Ruoran Li, a doctoral student in epidemiology at Harvard University, has been studying the epidemic in Wuhan for insight on how the outbreak might unfold in the U.S.
The Chinese government began by designating specific hospitals to treat COVID-19 and adding new beds to existing hospitals, Li says.
“They even built two new hospitals,” she says. “It still wasn’t enough.”
At the peak of the Wuhan epidemic, Li says over 2,000 patients needed intensive care in the city. Li analyzed what might happen if an outbreak like that happened in the United States. She and other researchers at Harvard published the analysis on the public online medical research archive MedRxiv.
“The result is quite sobering,” she says. “We maybe have just enough beds in the U.S. to treat critically ill patients from COVID. But that’s the total number of ICU beds in the U.S. If you think of all the [other] patients that need intensive care treatment at any point in time, the added needs from COVID patients could overwhelm the system.”
The analysis hasn’t been reviewed by independent experts yet, but it suggests that hospitals may need three times more ICU beds than they currently have available to keep up with the coronavirus.
At Tufts Medical Center, Doron says hospital leaders are ranking every possible location where they might place extra beds.
“It could be open spaces. It could be auditoriums or physical therapy treatment areas. It could be research areas. Things like that,” she says. “Part of pandemic preparedness is looking at every option and putting them in the order of preference.”
And beds may not be the only thing to run out if the outbreak unfolds as it has in other countries, Doron says. The supply of protective equipment, like fitted masks to shield healthcare workers from infection, is under strain.
“Hospitals around the country and around the globe are simultaneously increasing their supplies. So supplies might not be plentiful enough to scale up to a certain point if we want to get there,” she says. “So that adds an element of frustration to our preparedness.”
Doron says some hospitals have begun reserving fitted masks for procedures with the greatest risk for infection. Many hospitals are also winding down certain non-essential procedures – like some surgeries and outpatient services – to conserve supplies and free up medical staff to work in areas that may soon have greater need. On Sunday evening, Gov. Baker ordered all hospitals to postpone these procedures.
Over the weekend, two Massachusetts medical facilities reported employees had tested positive for the coronavirus, the first such cases in the state.
Doron says doctors at Tufts have begun giving each other crash courses in their areas of expertise so that others can step into new roles if necessary.
“It’s not just about getting sick,” Doron says. “It’s about getting exhausted.”
Medical staff have already seen an added burden simply with the preparation efforts around coronavirus.
“We haven’t necessarily been getting a full night’s sleep in the previous weeks,” Doron says.
If a surge of patients rolls into the hospital, that will stress health professionals even further.
But medical leaders are preparing for that, too. Boston Medical Center has been expanding resources to make sure health workers stay healthy and to help them cope with the pressure that may come in the coming weeks.
“This is a crisis that none of us have ever experienced before,” says Dr. Ravin Davidoff, the chief medical officer at BMC. “We have a deep commitment to our patients and to our employees to keep them safe. It’s taking up my entire day thinking and planning and talking about this. It’s our priority now.”
This segment aired on March 16, 2020.
