Advertisement
Coronavirus Coverage
Vaccines Will Take Months To Slow Down The Pandemic. Until Then, Mask Up
Traducido por El Planeta Media.
As coronavirus vaccines roll out, the temptation to relax COVID-19 precautions and restrictions grows ever more enticing. After all, some of us may already be immune. How good would it feel to have a hug just once in a while with a dear friend, or to free your nose from under the mask’s misty cover for a breath of cool, crisp air?
Well don’t.
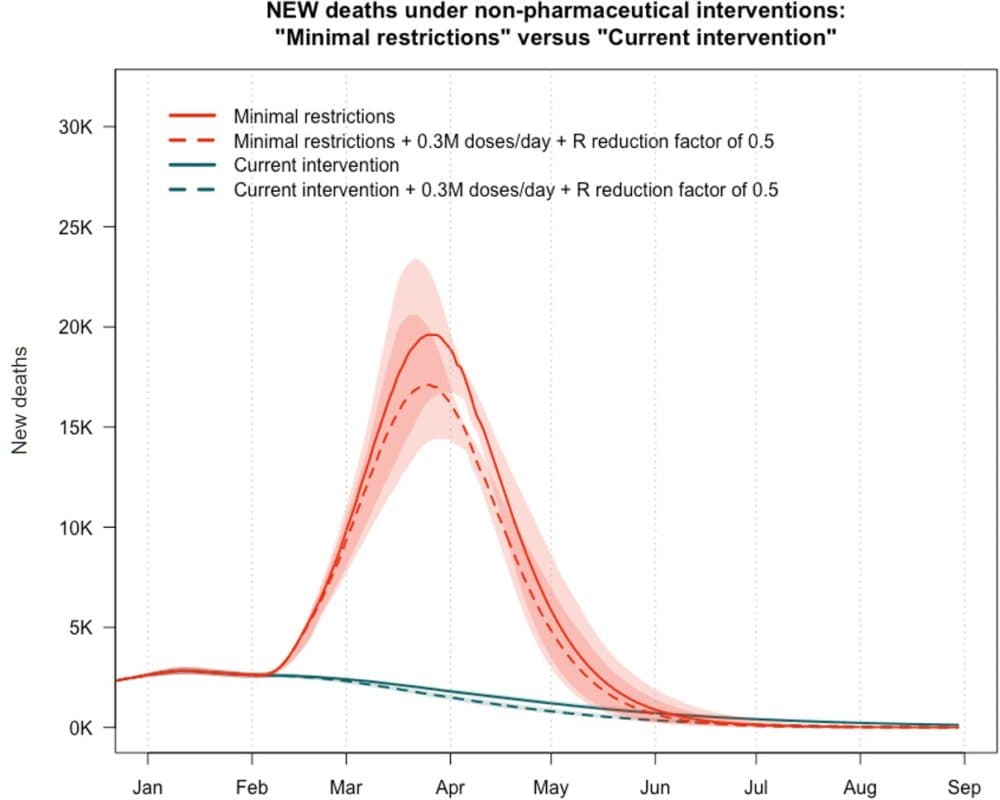
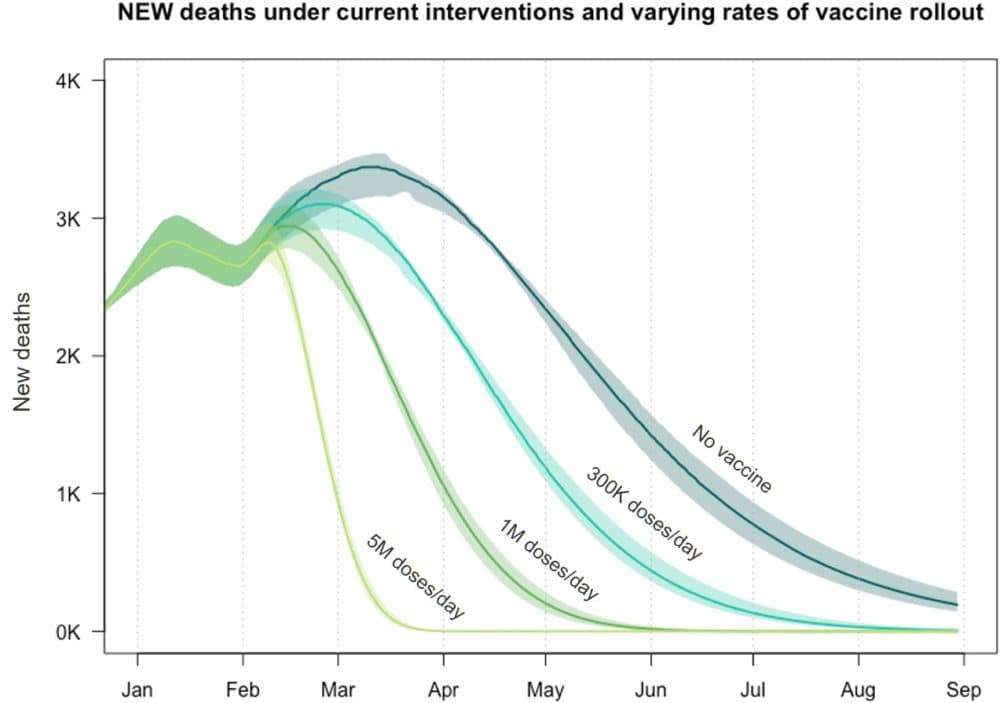
Vaccines may one day allow us to uncover our faces and bring the pandemic to an end, but they won’t do much to lower COVID deaths for at least the next few months, says Dr. Benjamin Linas, an epidemiologist at Boston University. According to statistical models he developed with colleagues from Massachusetts General Hospital and Georgia Tech, the number of lives saved by basic coronavirus mitigation measures — like masking, physical distancing and testing — are likely to eclipse the number of lives saved by vaccines over the next year.
That’s because it will take time for vaccines’ effect on the pandemic to be felt. At the moment, only about 7% of Americans have received at least one dose of the Pfizer or Moderna vaccine. Only about 6% of Massachusetts residents have gotten at least one dose, and it will be months longer still before a majority of the population is expected to receive a vaccine. Until then, Linas says, masks, distancing, testing and other basic mitigation measures are the only things really protecting people from COVID.
“That’s what’s saving us right now. The vaccines are doing nothing right now at a population level [for transmission]. Like, it’s just barely gotten out there,” Linas says.
At a hypothetical 300,000 vaccinations per day, Linas and his colleagues’ model suggests that the vaccines will only make a marginal difference in deaths for the next few months. Take masking and distancing away, and the model predicts the death rate would shoot up to over 15,000 deaths per day in April, even with the vaccines. With the emergence of more infectious variants like B.1.1.7, Linas says that number might be even greater.
Advertisement
“The reality is the vaccine is not a silver bullet. It’s obviously really important, but it’s not like, 'Yay we have the vaccine, all our problems are solved,' ” Linas says. “If you want to get to a world where we can start to loosen [restrictions] over the summer or next fall, put your masks on and don’t take them off.”
The model’s predictions are already playing out in one country where vaccinations are high but compliance with mitigation measures isn’t, says Dr. Shira Doron, a hospital epidemiologist at Tufts Medical Center. Israel is leading the world in COVID-19 vaccinations at the moment, but cases hit a new high this month.
“They’re vaccinating as fast as they can, way faster than anyone else in the world,” Doron says. “And yet their deaths are increasing. So yeah, [vaccinations] cannot work alone.”
Doron says that suggests vaccines aren't slowing the pandemic down, at least not yet. Only disciplined adherence to masking and distancing can do that right now. Even those who have already been vaccinated should not let their guard down, Doron says. Since the vaccines are effective in 95% of people who receive two doses, that still means one out of every 20 people won't become fully immune to the virus.
“Even when vaccinated, with a huge number of cases there’s still a huge sort of risk around you,” Doron says. “Even the vaccinated people need to keep doing the mitigation measures, or they’ll be part of the problem.”
Time is also of the essence, Linas says. Of course, the sooner people are vaccinated, the quicker they're protected and deaths will begin to drop. But with the emergence of the more infectious variant B.1.1.7, Linas says more variants are certainly on their way. If only part of the population is vaccinated, then the virus has a greater likelihood of evolving — and in ways that may evade the vaccine's defenses.
"If you go through a long period where some are vaccinated but not everyone, and there's still ongoing transmission, that's when viruses start to mutate and skip the vaccine," Linas says. "If everyone is vaccinated, the virus extinguishes. So that's another reason we have to go fast. Faster is better."
