Advertisement
Asthma's Up, Yes, But Are Distorted Financial Incentives Still Driving Care?
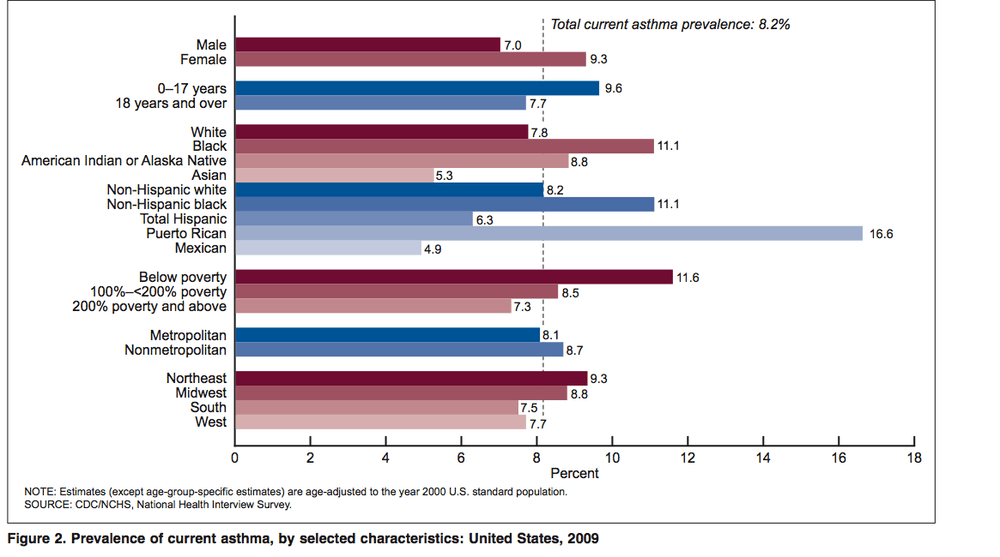
The CDC reports that nearly 25 million Americans, or 1 in 12, now suffer from asthma. That's a prevalence rate of 8.2 percent in 2009, up slightly from 7.7 percent in 2005. Asthma rates tend to be higher among certain groups: women, children, blacks, the poor and people who live in the Northeast and Midwest. (A report last year found that New England asthma rates are highest in the country.)
But according to David Link, Chief of Pediatrics and head of the pediatric asthma program at Cambridge Health Alliance, higher asthma rates are a non-story. "Asthma is steadily rising in every developed country and has been for years, ho hum," he says. "The real story is, what the hell is wrong with us, the medical community, why don't we do what we can do to prevent this? We can't make the asthma go away, but we can make the unscheduled visits to ER and admissions to the hospital go away."
Dr. Link has written previously about the distorted financial incentives driving asthma care. He says the ubiquitous respiratory illness is generally a big profit generator at hospitals, which makes promoting prevention very tricky. But what may be costly for a specific hospital, he says, would generate huge savings to society.
"Step into any pediatric ward in the region and you will find that asthma-related treatment is most likely their number one cause of admission and source of revenue," Dr. Link writes. "Because of these powerful financial incentives, it has been difficult to reduce asthma related admissions and emergency visits in favor of prevention. In fact, there are significant additional resources required for prevention and better disease management which are not reimbursed, hence the failure to obtain any serious traction here."
Here's Dr. Link's piece on the skewed incentives behind treating asthma, written in May, with Cambridge Health Alliance CEO Dennis Keefe:
The findings in a recent report from the Asthma Regional Council of New England were unsurprising but nevertheless disturbing. Quite simply, New England asthma rates are highest in the country and we don’t seem to be making much progress in lessening this scourge. With 1.3 million people in the region suffering with asthma, an amount that has increased by 100,000 since 2001, asthma not only afflicts individuals – it is a common cause of death in our region – but also contributes mightily to lost productivity, absence in the classrooms, rising health care costs, ballooning workers’ compensation expenses and many other associated negative outcomes.
Experts like to debate why New England is so unequally affected – our old housing stock, the fact that we are at the end of the jet stream and other environmentally unique factors are no doubt involved – but there is an oft-overlooked factor that presents significant obstacles to reducing the burden and cost asthma brings to patients and populations: For one, Asthma is a big revenue generator for hospitals. Prevention, on the other hand, is not. Step into any pediatric ward in the region and you will find that asthma-related treatment is most likely their number one cause of admission and source of revenue. Because of these powerful financial incentives, it has been difficult to reduce asthma related admissions and emergency visits in favor of prevention. In fact, there are significant additional resources required for prevention and better disease management which are not reimbursed, hence the failure to obtain any serious traction here.
It’s not the fault of hospitals and health care providers. In general, our health care payment system provides no financial incentives for prevention. In our current through-the-looking glass health care model, what is good for populations and public health is unconnected to what is good for providers and health care delivery.
Asthma is a serious public health problem and needs to be dealt with in a population-based, public health manner, much like our state’s Immunization Initiative, in which vaccine-preventable diseases are tracked and care is dispensed according to need under established guidelines.
The first step in resolving this – after simply acknowledging that asthma is indeed a public health issue – is to compile data at the population level and build a registry to collect and use the data for tracking outcomes, measuring progress, and reporting to providers as well as public health agencies.
We know from personal experience that such a system will work. Cambridge Health Alliance has maintained an on-line registry for children with asthma that was launched in 2002 with the help of funding from the Robert Wood Johnson Foundation. It is the centerpiece of a multi-disciplinary, planned model of care for patients with chronic illness and involves pediatric and family medicine practices, planned care coordinators, parents, school nurses, healthy homes assessments and access to the registry where each child’s current care plan is available to all providers and units in our network. More than 3,000 children with asthma are followed, and we are now developing a similar system for ADHD.
Since 2002 we have seen a 45 percent decrease in inpatient asthma-related admissions (from 4.8 percent to 2.6 percent) and a 50 percent decrease in ED visits (from 17 percent per year to 8.5 percent) by this population. Integrated technology systems to support all this is essential, similar to the immunization registry, and helps provide a framework for alignment to reach goals and provide real-time feedback – not 60-to-90 day lags – to quickly understand how progress is proceeding and what methods work best.
Organizing care this way – according to established guidelines and communicating among all providers and community resources – is not cheap. And our current payment system simply does not recognize these costs. There’s no reimbursement model for outreach, non-traditional encounters, telephone counseling and other simple methods of preventive medicine. That’s why it is important that prevention be a centerpiece of the health care payment reforms now being developed by the state and federal governments.
Even then, it may be a challenge to demonstrate how preventive efforts can save us money and how to incent institutions toward a prevention model. We know from our own experience that a $250,000 estimated annual investment saves payers – Medicare, Medicaid and private insurers – an estimated $800,000 every year in ED visits and inpatient costs. Payment reform must build in methods to share those savings with providers, or at least recognize and pay for the cost of the necessary prevention systems.
Without support from the insurance industry, governments and private foundations, there’s no way to convince a hospital administrator that severely reducing the volume of asthma patients that visit each year will be good for the bottom line.
Currently, there is a Medicaid Global Payment Demonstration Project for asthma included in the House budget. If we’re really interested in seeing declines in this terrible disorder, it should win unanimous support.
Note: Dr. Link says this asthma global payment demonstration project is now pretty much off the table but he's working on a related national pilot project. Stay Tuned.
This program aired on January 13, 2011. The audio for this program is not available.
