Advertisement
Coronavirus Coverage
Mass. Plan Swaps Hospital Competition For Collaboration As COVID-19 Surges A Second Time

In the spring, as patients with COVID-19 poured into Massachusetts hospitals, an unusual, ad hoc collaboration kicked in. Boston Children’s Hospital took in kids from other institutions that needed more space for adults. Hospitals loaned ventilators and other equipment to competitors. And they handed over vials of scarce meds.
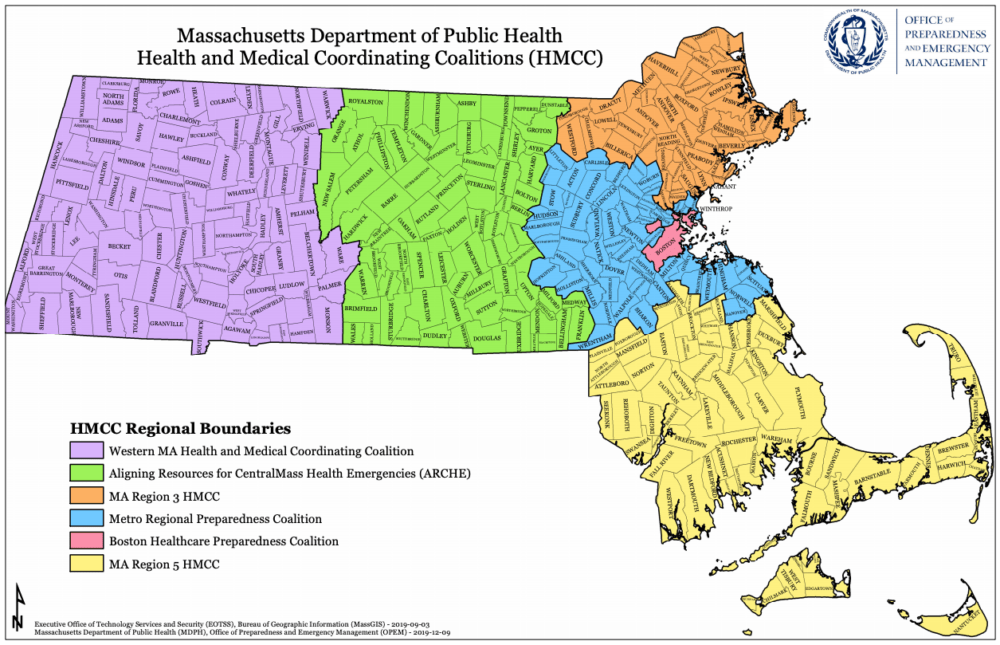
Now, with agreement from the Massachusetts Health and Hospital Association (MHA), the Baker administration is turning those informal arrangements into a formal, regional plan. Hospitals, grouped into five areas, will meet at least weekly to share updates about their bed capacity, staffing levels, PPE and other supplies, and ability to accept transfer patients.
The goals are to avoid having any one hospital or region become overwhelmed by a spike in cases, to continue elective and non-urgent care, and to make sure patients in every part of the state have equal access to the best possible care.
Gov. Charlie Baker says he does not want to stop routine care for adults or children, which happened during the first surge, so that hospitals could reassign beds, equipment and staff to COVID patients.
“Those resources are finite,” Baker said Tuesday. “We don’t want to go back to the restrictions we put in place last spring.”
This regional approach could be put to the test soon. Hospitals leaders within each region begin meetings this week. Many hospitals in Massachusetts are close to full with patients who postponed care, an emerging flu season and rising cases of COVID. The Baker administration says COVID hospitalizations are up 200% since Labor Day.
“So this time around with COVID, a smaller number of COVID patients could cause as much clinical disruption now as before, even though the circumstances are quite different,” said Dr. Richard Nesto, the chief medical officer for Beth Israel Lahey Health.
The two largest hospitals in the Beth Israel Lahey Health network are already at 95% capacity, Nesto says.
What’s different this time, Nesto says is that hospitals are better prepared and have a better understanding of how to treat COVID. And hospitals don’t expect this surge or ones to follow will be as steep as the first one in April.
But if hospitals plan to manage new waves of COVID patients while taking care of all their other patients, leaders say they need this regional plan. One hospital might stop performing colonoscopies or heart monitoring tests or some elective procedures for a short period of time and let other hospitals in their region or outside take those patients.
“This is what is really important about the state’s approach and is fundamentally sound. Each hospital may run a little bit differently,” said MHA president Steve Walsh. “This [regional plan] allows some flexibility.”
The state will monitor capacity in each region and may shut down non-urgent care, regionally, if more than 80% of beds are full for a week or longer.
Walsh says this regional plan is based on the understanding that waves of COVID patients are not uniform across the state. In the spring, for example, Berkshire Medical Center filled early with COVID patients, but then was almost empty as the surge moved to Boston and elective care was still suspended.
Hospitals across the country are transferring COVID patients as the pandemic reaches another critical stage. Moving patients who need specialized care is not new, but mass transfers can be complicated, says Dr. Eric Wei the chief quality officer at New York City Health and Hospitals. Wei and colleagues described lessons learned about so-called “level loading” during the first surge.
Wei says New York does not have regional or statewide plans.
“The dream would be to do that across the city and state,” Wei said. That level of collaboration “will lead to better care and higher quality care.”
The American Hospital Association says several states including Utah, Kentucky, Alabama and Nevada have plans in place that encourage or facilitate collaboration between hospitals.
The hope in Massachusetts is that regional cooperation will reduce disparities between hospitals, especially those that serve low-income patients who are more at risk for infection and hospitalization than higher income patients.
But asking hospitals that compete, sometimes fiercely, for patients, to work as if they are all part of the same network is still a work in progress in Massachusetts and beyond.
“Eastern Massachusetts is a highly competitive health care market,” Nesto said. “But what we discovered in March and April is that we’re not competing. We’re trying to take care of an avalanche of patients.”
Now hospitals will see if they can maintain that spirit with more formal rules in place.
