Advertisement
Coronavirus Coverage
Many Mass. hospitals are short-staffed. The culprit may not be a shortage of nurses
Traducido en español por El Planeta.
There’s a lot of talk about a shortage of nurses and other hospital staff during the pandemic, a shortage that means patients sometimes wait in hallways until a bed opens up, or have to reschedule surgery. But state numbers show there are more licensed nurses now, in almost every category, than before the pandemic.
The state Board of Registration in Nursing shows a 24% increase in licensed registered nurses this month as compared to June of 2019. And that’s in addition to nearly 12,000 temporary — or travel — nurses licensed during the pandemic. So, why do many hospitals, community health centers and clinics have job openings?
The state’s main nurses union says the answer is not because there’s an actual shortage of nurses.
“It’s a shortage of nurses willing to work under these conditions,” says Katie Murphy, president of the Massachusetts Nurses Association.
Conditions that many nurses say leave them in tears or unable to function immediately after a shift. While the state doesn’t track how many of the nurses on its rolls are currently employed, many nurses describe leaving jobs they once cherished in the wake of COVID and its ripple effects.
Why Nurses Are Leaving Hospitals
Carrie Pessini remembers arriving for work at an emergency room a few months before she quit. A colleague briefed Pessini on her patients, including a young man with a heart condition.
“When I go in to assess that particular patient, he was not responding,” Pessini says. “Unfortunately, that patient had experienced a possible opioid overdose.”
Drug overdoses are up during the pandemic.
“I truly do not think, right now, that people can be a bedside nurse for their entire career. It is not physically, emotionally or spiritually possible.”
Carrie Pessini
While Pessini used naloxone to revive the man, she could see another patient oozing blood from their temple. A man strapped to a stretcher rolled in having an emotional breakdown.
ERs are busy places, but Pessini says the pace became relentless. She would leave the hospital a wreck, sometimes unable to speak for several hours.
“In your eight to 12 to 16 hour shift, you don’t have time to process anything that you’ve experienced,” Pessini says, “whether it’s a multitude of patient deaths or a mother screaming because her child is really sick or might have passed away. The sounds of everything that rings in that department, you take home with you.”
Pessini resigned to work at a mobile psychiatric program. She says she’s one of many veteran nurses who are trading jobs inside hospitals for positions that are less stressful and more rewarding.
“I truly do not think, right now, that people can be a bedside nurse for their entire career,” Pessini says. “It is not physically, emotionally or spiritually possible.”
Advertisement
Amy Smith, another former emergency room nurse, would have disagreed with that statement before the pandemic. But about this time last year, Smith found herself in tears before every shift. Smith says she’d wake up, realize it was a work day and slip into “a really heart-felt defeat.”
Smith’s feeling is captured in her memory of an elderly woman on a gurney in a hallway, smeared with feces and urine. Smith had seven other patients that shift. She had to prioritize two who needed round the clock intensive care. So it was three or four hours before Smith cleaned the woman.
“It weighed, huge,” says Smith, describing that shift and the weeks that followed. “It’s helplessness and hopelessness all at the same time, with no end in sight.”
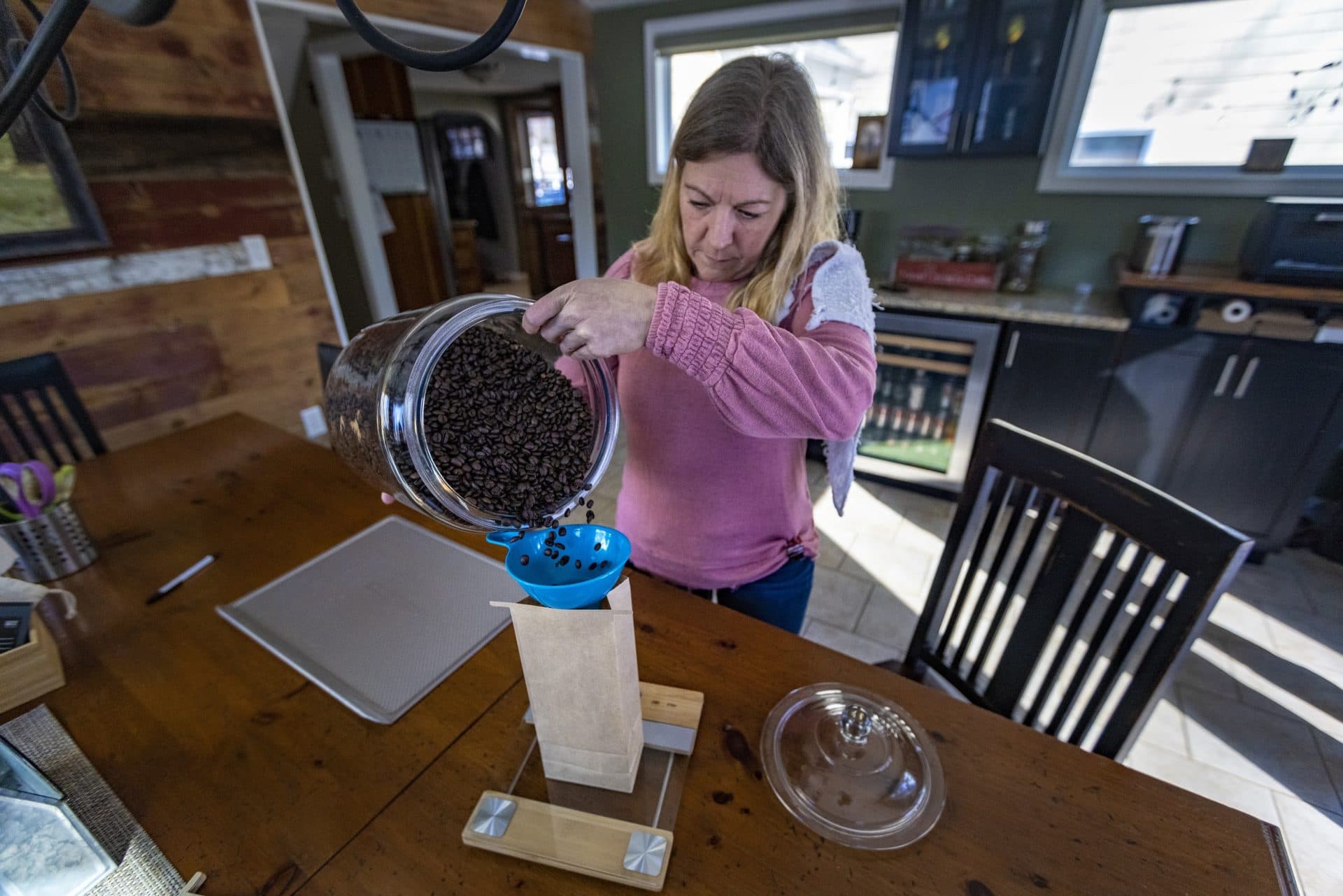
Smith quit in November 2021, taking 25 years of expertise with her. She’s roasting coffee beans now, hoping to open a cafe where she can look people in the eye, ask about their lives and offer comfort, things she loved in earlier years as a nurse.
Difficult working conditions are not the only reason RNs are leaving. Some have been out sick with the virus. Most returned, but others are out on long-term disability. Some nurses with young children cut their hours or are on leave because daycare and schools have been unpredictable. And there are nurses who decided not to return after they were laid off early in the pandemic.
Nurses are also among a small portion of hospital employees fired for failing to get COVID vaccines. Katelyn, who’s been an ICU nurse for 13 years, says she asked the hospital where she was employed for a medical exemption but was denied. We’ve agreed to only use her first name.
Now, Katelyn is a travel nurse, moving from one hospital to the next within Massachusetts. She says the agency that books her jobs and the hospitals where she works have accepted her request for a vaccine exemption. She doesn’t know how long this phase of her nursing career will last. Katelyn says some of the hospitals that rely on travel nurses have terrible working conditions.
“I thought the position I was in before was draining but this is just awful,” she says. “And I don’t know if I can go through the stress every 13 weeks of trying to find my next contract.”
Katelyn says hospitals in crisis mode are still offering good pay, $100 an hour or more, but others are cutting the travel nurse rate in half or canceling contracts with these temporary nurses as hospital crowding eases.
Efforts To Retain Nurses, New Elements For Those In Training
The Massachusetts Health and Hospital Association says retaining nurses and addressing burnout is a top priority. MHA’s vice president of clinical affairs, Patricia Noga, says many hospitals are offering more flexibility.
“It’s really working with the individual nurse to see what would be more helpful to them in terms of staying in the workforce,” says Noga, which may mean letting nurses choose their hours, the days of the week they want to work and where in the hospital they want to be assigned.
Many nurses talk about two other changes that might help keep them in the job. One is limits on the number of patients they’re assigned. A ballot question that would have established such nurse-to-patient ratios was defeated in 2018 after a bruising fight between the hospital association and nurses union.
In the aftermath, the MHA launched a task force that released a report late last year, Caring for the Caregiver. It talks about the importance of safe and effective staffing but does not recommend specific patient limits for nurses.
The second request from many nurses is more money to acknowledge their increased stress. Noga says some hospitals are providing financial assistance for childcare. Others are adjusting wages based on the demand for nurses.
“Some of that is beginning to happen,” Noga says. “Where it’s going to go, I’m really not sure.”
Many people are reassessing what they want from a job during the pandemic, with nurses and other health care employees at the forefront, says Rachel Lipson who directs the Project on Workforce at Harvard. Lipson co-authored a report, COVID-19 and the Changing Massachusetts Healthcare Workforce, released in September 2021.
“I feel somewhat encouraged that there’s at least conversations happening about how do we make this a more sustainable profession,” Lipson says. “It’s not just about the ratios on the floor but we do need some rethinking of the role, what the job looks like and the whole person that fills these jobs.”
“Sometimes I would lose sleep over the tasks I didn’t get to.”
Juanita Saenz
During the pandemic, the state allowed nurses from out of state or who had let their licenses expire to activate them immediately under a public health emergency order issued in November 2021. Those licenses will expire in June of this year. Nursing licenses typically come up for renewal every two years.
To create a pipeline of nurses inside hospitals, some are helping medical or nursing assistants get the education and training they need to become nurses. Noga says hospitals are working closely with nursing schools on these programs.
Rosanna DeMarco, interim dean at UMass Boston’s nursing school, says developing these partnerships will help her students get more clinical experience, and they’ll expand the pool of teachers, which UMass Boston needs as fewer nurses join nursing school faculties.
DeMarco says enrollment is up. But students hear the stories about nurses leaving and are afraid of the work environments they may enter. In response, DeMarco has added sessions this year on how to manage stress, find a mentor and develop peer support networks.
“It’s not just about ‘this is how you take care of the patient, here are the tools,’ ” she says. “It’s about the mental set-up that one needs to have to work with patients now that needs really to be addressed in a very direct and formidable way.”
Stress Across The Nursing Landscape
The conversation about nursing shortages often focuses on hospitals, but clinics, community health centers and home-care agencies are all struggling to retain nurses and fill vacancies as well. The decisions of two sisters in Boston, Juanita and Tatiana Saenz, highlight the challenges.
Juanita Saenz got her first job as a nurse in January 2020, at a community health center. She made it through the first year of the pandemic, then quit to work at another community health center closer to where she lives. Much of the care was remote. Juanita says she soon got tired of hearing frustrated patients yell at her. And she felt like her day was controlled by the center’s electronic medical record system and its relentless demands.
“Sometimes I would lose sleep over the tasks I didn’t get to,” Juanita says.

She left that center to work at a clinic where travelers get the shots they need for international business trips or vacations. Juanita says she has a manageable number of appointments now, with pleasant clients, and she can take care of personal business during the day when needed.
“There’s a huge shift with younger people realizing that they’re a person first before a worker,” she says.
Her sister, Tatiana Saenz, recently handed in her notice at a community health center where she says she feels overwhelmed most days.
“It is a pressure in my chest,” Tatiana says, holding her fist to her sternum. And she says her brain fogs. “You forget people’s names despite asking for them three or four times in the same day.”
Last fall, Tatiana realized she couldn’t recall some conversations with patients from one day to the next. She took a three month leave then returned to work, but still feels beaten down. Here’s one reason: she’s tired of the daily fight to find mental health or substance use treatment for patients who need it.
“It’s that inability to feel confident in telling them that tomorrow’s going to change when in reality I don’t know any more,” Tatiana says.
When she leaves in April, after nearly a decade in hospitals and health centers, Tatiana plans to go back to school full time. She wants to finish a masters in nursing informatics so she can stay involved in the profession but focus on data instead of direct patient care.
“It wasn’t an easy decision to make,” Tatiana says, “but at the end of the day, I don’t want my body to pay the price for continuing doing the work that’s stressful for me and affects my mental health.”
This segment aired on February 28, 2022.
