Advertisement
Why are cancer rates rising among young people?
Resume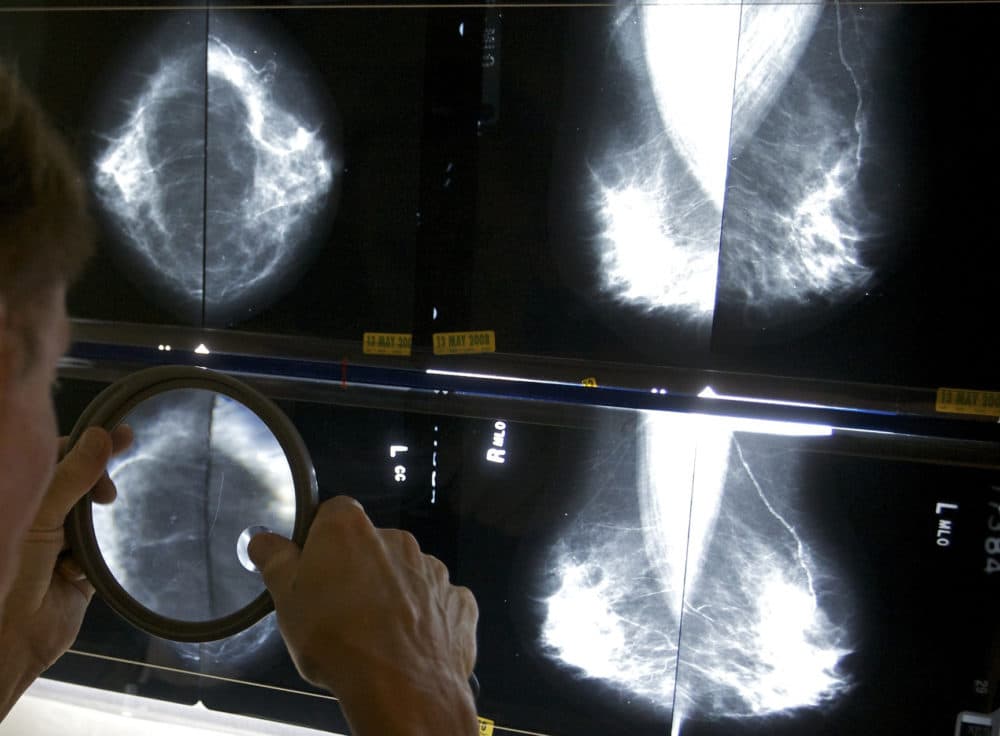
There's a troubling trend in medicine — increasing cancer diagnoses in people younger than 50.
"Seeing somebody in the prime of their life, in the height of their career, having young children, being hit with an advanced terminal diagnosis like this is what keeps me up at night," Kimmie Ng, director of Young-Onset Colorectal Cancer Center at Dana Farber Cancer, says.
So what’s to blame for rising cancer rates among young people? Is it diet? Lack of exercise? Environmental chemicals?
"They’re again actively trying to dismiss concerns about the chemicals that they produce and use," Julia Brody, executive director and senior scientist at the Silent Spring Institute, says.
Today, On Point: What we know — and what we don’t — about early-onset cancer.
Guests
Dr. Kimmie Ng, director of Young-Onset Colorectal Cancer Center at the Dana-Farber Cancer Institute.
Dr. Tim Rebbeck, Vincent L. Gregory, Jr. professor of cancer prevention and epidemiology at Harvard T.H. Chan School of Public Health.
Also Featured
Alexa Morrell, mother diagnosed with Stage 4 colon cancer.
Dr. Laura Esserman, surgical oncologist. Professor of surgery and radiology and director of the multidisciplinary breast cancer program at the University of California, San Francisco.
Dr. Julia Brody, executive director and senior scientist at Silent Spring Institute.
Dr. Peter Campbell, professor of epidemiology at Albert Einstein College of Medicine.
Transcript
Part I
MEGHNA CHAKRABARTI: In the fall of 2019, Alexa Morrell, a busy working mom with a one year old at home, took a weekend getaway to Cape Cod, Massachusetts.
ALEXA MORRELL: It was the first weekend away from my son with my friends for a girls weekend. So it was really just like a fun time to just take my mom hat off, like it was a weekend of laughing, going to the beach and going out to eat.
CHAKRABARTI: Well, it didn't really turn out like that, because Alexa began noticing something was wrong with her body. There was blood in her stool.
MORRELL: It was on and off for almost two weeks, and then at the end of two weeks, it was a lot of blood, and at that point, I made a mental note, like, "Okay, if this doesn't go away in two weeks, I'm going to go to the doctors."
CHAKRABARTI: Alexa did eventually have to go to the doctor. Her primary care physician thought it was probably hemorrhoids, not a huge deal, but ordered a colonoscopy just in case. That colonoscopy led to a CT scan the next morning, which led to an agonizing wait.
MORRELL: I kept calling the hospital to see if there was any update, and at 4 p.m. is when I got the news that unfortunately not only do they see a tumor in my colon, so essentially colon cancer, so I, at that point, I didn't think it was going to get any worse, and then he kept talking and said, "Well I also see it in your liver.
And so sorry, this means that you're Stage 4." We were told that I had Stage 4 cancer as I'm holding my 13-month-old in my lab. So it was just like an out of body experience, is the only way that I can describe it. I was just like in complete shock and disbelief, that will always stand as the worst day of my life.
CHAKRABARTI: Alexa was just 29 years old.
This is On Point. I'm Meghna Chakrabarti. This wasn't supposed to happen, of course. Alexa was building a family and a career. She had a plan. A plan that did not have room for Stage 4 colon cancer. And did not have room for spending long days at the hospital. But suddenly, there she was.
MORRELL: I was recommended to do really strong chemo for colon cancer, which going into it knew that it was possibility of me losing my hair.
And I did lose it, which was really hard.
CHAKRABARTI: Then came the surgeries. Alexa has 65% of her liver removed, her gallbladder removed. Then even more. of her liver removed, 12 inches of her colon removed, the middle lobe of her right lung. She's had radiation treatment, too. So it's been a long road for Alexa and for her family.
MORRELL: When you get diagnosed, they tell you not to Google the statistics and odds. I don't even want to say it because it's not good, but the chance to live five years after this diagnosis for Stage 4 is really slim. So to be here four years later. It's keeping me very hopeful. I'm really happy to report that I have made 20 months clear in my lung and 40 months in my colon and liver.
And I have scans in two weeks, and this would make my sixth consecutive clear scan in a row, if they're good. So I am feeling more hopeful as I continue to stack up more clear scans in a row. A lot of people with this disease don't always do well. So I know I'm one of the lucky ones and I really don't take it for granted at all.
CHAKRABARTI: Alexa is 33 years old now. Her son, who was just over a year old when she was diagnosed, is now five.
MORRELL: I remember getting diagnosed and being like, "Oh my God, am I going to even see him go to kindergarten?" So to just check off that milestone a couple weeks ago just felt so good. It was like such a full circle moment that like, I'm like, "Okay, on to the next milestone, like fifth grade graduation and, you know, high school graduation."
And so dreaming like bigger milestones as I kind of check off smaller ones. It feels really good to be able to do that.
CHAKRABARTI: Alexa's getting on with her life. She works full time, she just returned to her Orange Theory fitness classes, but she says cancer is never far from her mind. Because she knows that each new scan could turn everything upside down again.
Stories like Alexa's are becoming more common. While overall rates of cancer in this country have fallen in recent decades, the rate of cancer diagnosis in young people, we're talking people below the age of 50, is increasing. Rates of early onset colorectal cancer have doubled since the mid 1990s, and doctors and researchers are working to figure out why.
So today, we're not just going to talk about colorectal cancer, but all forms of cancer, and why, as I said, we are seeing an increase in early onset cancers. And I'm going to start today with Dr. Kimmie Ng. She's director of the Young Onset Colorectal Cancer Center at Dana-Farber Cancer Institute in Boston, Massachusetts.
Dr. Ng, welcome to On Point.
KIMMIE NG: Thank you for having me.
CHAKRABARTI: Now, I should say that Alexa, because she received some of her treatment at the Dana-Farber Cancer Center. How common or familiar is a story like hers amongst the patients that you see?
NG: It is really typical of so many of the unique challenges that we are seeing when a young person is diagnosed with cancer.
Don't get me wrong. It's difficult to get a diagnosis like this, no matter what age you are. But we do know that young people face unique challenges. They're in the prime of their life, they're family planning to have more children or and they want to start having children. They're in the middle of their careers.
They're also maybe taking care of their elderly parents. It's really the sandwich generation and to be hit with a diagnosis like this has an unusual toll and it's just devastating for a young person.
CHAKRABARTI: I was hearing Alexa say that just in case her doctor, her primary care physician, after she noticed those, that first sort of trouble with her body, just in case ordered a colonoscopy.
Now remind me. At this point in time, what is the recommended age for regular colonoscopy screenings?
NG: So in direct response to these rising rates of young onset colorectal cancer, the United States Preventive Services Task Force changed in 2021 their guidelines to recommend that people at average risk start screening at age 45 now instead of 50.
So the new age is 45 for people who are at average risk.
CHAKRABARTI: Okay, so they've dropped it down a little bit.
NG: They have.
CHAKRABARTI: About five years. But Kimmie, sorry, I keep doing that, forgive me, Alexa was 29 when she got her diagnosis. Are you seeing, in the young onset colorectal cancer center, are you seeing patients that young or even younger?
NG: We are, unfortunately. So those statistics are reality. We see day after day, week after week. 20-year-olds, 30-year-olds, 40-year-olds with no family history, no genetic syndrome, no risk factors following a healthy lifestyle who are being diagnosed with advanced stages of colorectal cancer.
CHAKRABARTI: Advanced stages?
NG: Yes. Unfortunately, the majority of these young people are diagnosed with Stage 3 or 4 cancer, which is much less curable than if it were diagnosed at Stage 1 or 2.
CHAKRABARTI: Wow. Okay. So how different is this in terms of the rates or frequencies that you're seeing? And we'll stick with colorectal cancer here for another few minutes.
Then we were seeing, I don't know, 20, 30 years ago.
NG: Yeah. So the rates of young onset colorectal cancer, so colorectal cancer in people under the age of 50 have increased by about 2% per year since the mid 1990s. And cancer deaths in these young people have now also started to rise. And this is very different from a few years ago.
This increase follows a birth cohort effect where the change is varied by generation. A person born in 1990 now has quadrupled the risk of developing rectal cancer compared to a person born in 1950.
CHAKRABARTI: Wow, okay. Now, I always want to be careful in talking about relative risk versus absolute numbers. Because while we're seeing a rise in the rate, can you tell me a little bit more about in terms of overall numbers?
Are there still more people over the age of 50 who are receiving these diagnoses than younger people?
NG: Yes, no question about it. People over the age of 50 are at much higher risk of developing colorectal cancer. And it's important that we get all of those people definitely screened. So the absolute numbers of young patients is still relatively small.
However, it is steadily increasing, and the rate of rise is steepest in the very youngest, in their twenties and thirties.
CHAKRABARTI: Okay. So nevertheless, it is cause for concern. And then before this It's sort of roughly 1990-ish mark, let's put it that way. Or do we have adequate studies in terms of what the rates of early onset colorectal cancer were prior to that?
NG: Yes. Way back then, probably less than 10% of all colorectal cancers were diagnosed in young people and now it's probably 15% or more. And we now estimate that by the year 2030, colorectal cancer is going to surpass breast cancer to become the leading cause of cancer death in people under the age of 50.
CHAKRABARTI: Okay. Wow. So this isn't necessarily in terms of this kind of cancer. It's not necessarily, we're screening more, so therefore we're catching more.
NG: No, because if this were a screening effect, it would. So first of all, only people 45 and older get screened. And that was just a recent change.
But if this were a screening effect, we would be picking up more early-stage cancer.
CHAKRABARTI: Versus the 3 and 4 stage.
NG: Yes.
CHAKRABARTI: Okay. Oh, wow. Well, I have to tell you, Dr. Ng, this is one of those shows that when we let listeners know that we were going to be talking about it, we really received a flood of calls and messages.
So there's definitely something going on. Not that our program, number of calls is a scientifically accurate statistic, but it's remarkable, I think, nonetheless. So we're going to be hearing a lot of stories from various listeners throughout the hour. Here, for example, is one from Natalie, who's from Bainbridge Island, Washington.
She was diagnosed with Stage 4 colorectal cancer when she was 38. And as a mother, she told us it's very difficult to balance her own health needs with the needs of, you know, being a mother to her children.
NATALIE: There have been times when I have to focus on my own health, which means locking myself in a bedroom and not doing story time.
And then there's other times when I've had to get up in the middle of the night and change diapers connected to a chemotherapy pump. I've had to manage my children's anxiety around my health, which has always been a careful dance. Do I tell them I'm terminally ill? Do I wait till I go to hospice? Do I just tell them we're working on things and hoping to get better. I've been even careful to use the word cancer because I know that my older child who's now six, that word provokes anxiety.
CHAKRABARTI: You know, Dr. Ng, I'm thinking about how when a parent communicates that they're unwell to their child, the look of sheer terror on a child's face because, you know, the family, adults in the family are everything to that kid.
So how much, given that we are talking about people in their 40s, how much does managing the overall effect of the cancer diagnosis matter in the treatment of these younger people?
NG: It matters tremendously, just as much as the medical care of their cancer. And so when we were seeing young person after young person walking through our doors, we realized we need to take better care of these young people comprehensively, not just them, their whole family, because this diagnosis impacts the entirety of their circle.
So we started our young onset colorectal cancer center to do just that.
CHAKRABARTI: As I said before, we received so many calls and stories from people across the country who have personal experience with this. I want to share a few more of them. This is Michelle Davis. She's in Vancouver, Washington, and she was diagnosed with thyroid cancer at the age of 37 when her dentist found a lump in her throat.
She had her thyroid removed, along with the lymph nodes around her neck where the cancer had spread, and now Michelle takes synthetic thyroid hormones daily.
MICHELLE DAVIS: And I think about how it's changed my life, because not only do I have to take a pill every morning, But if something were to happen as far as like supply chains, it would be a big problem if I didn't get that medication. And within a few weeks, I would actually die if I didn't have that medication.
It was definitely a shock to have this cancer so early in my life. Nobody else in my family has a history of cancer. And when the doctors were kind of going through the process of diagnosis with me, a lot of their questions had to do with environmental exposures. Like if they wanted to know if I'd ever been to Chernobyl or other places like that, which I thought was so interesting because I hadn't.
But yeah, I had cancer when I was 37. Right now I'm 43. I'm in full remission and it was pretty shocking to have it at such a young age. It impacted my fertility. It impacted everything.
CHAKRABARTI: That was Michelle Davis in Vancouver, Washington. And here's Kirsten Salpini of Durham, North Carolina. She got a surprise cancer diagnosis as a college student.
KIRSTEN: I am 32. I was diagnosed with thyroid cancer at 21. And it was a surprise. I'm a singer and it was affecting my vocal cords, which is how we found it. But it's completely changed my life. I had a complication with the surgery, that affects me daily. It's made me more aware of my body and my health and not to take it for granted, like so many other really young people do.
And I had to grow up really fast. In college, having to manage something like that. But I do wonder why I got sick so young. Doctors said, you know, it was hard for them to believe. But thanks for doing this story. And this has helped me connect with other young people who have struggled with serious health issues in their 20s.
CHAKRABARTI: Again, that was Kirsten Salpini in Durham, North Carolina, and we will be hearing more stories from listeners throughout the hour. Well, I'd like to bring Dr. Tim Rebbeck into the conversation. He is a professor of cancer prevention and epidemiology at the Harvard T. H. Chan School of Public Health. Dr. Rebbeck, welcome to On Point.
TIM REBBECK: Thank you for having me. Great to be here.
CHAKRABARTI: So Dr. Ng got us started by talking about the dramatic rise in colorectal cancers in young people. Are we seeing a similar rise in other forms of cancer?
REBBECK: We are, and there are at least 14 cancer sites that have been increasing in incidence and mortality over the past 30 or so years.
So this is not a phenomenon limited to colorectal cancer. It's something that seems to be broader, across many sites for cancer.
CHAKRABARTI: Okay, so 14, we've heard already about colorectal cancer. Those listeners who sent their stories talked about thyroid cancers. Can you name a couple of others then?
REBBECK: Sure. Breast cancer, uterine or endometrial cancer, esophageal cancer, gallbladder cancer, kidney cancer, liver cancer, pancreas, prostate, stomach, there's quite a few. And really, across many different organ systems, and for cancers that are really very heterogeneous in terms of the risk factors and the things that we think are causing cancer in general.
CHAKRABARTI: Okay, we're going to come back to those other forms of cancer, but Dr. Ng, let me ask you something. Because several of the ones that Dr. Rebbeck just mentioned were gastrointestinal essentially. And I'm seeing some studies, for example, there was a recent one in the Journal of the American Medical Association, that followed, did a cohort study of more than 500, 000 patients. And they were younger than 50 and found that the majority of those cancers were gastrointestinal.
Is there any reason why you think that might be?
NG: Yes. So a lot of these rising early onset cancers are digestive system cancers. And some of them may share similar risk factors with the leading hypothesis being obesity. Many of these cancers are associated with obesity. And as we know, in recent decades, the rates of obesity have skyrocketed dramatically.
CHAKRABARTI: Okay. And Dr. Rebbeck, what do you think about that?
REBBECK: Yeah, that's the leading hypothesis right now. It's interesting that some of the cancers that are early onset increasing are also the obesity related cancers. So if you line them up next to each other, they align pretty well. And so there is clearly something going on.
And many of the cancers, there's plenty of good research right now showing that early onset cancers are associated with obesity. So I think that's probably our leading hypothesis. But of course, there are others.
CHAKRABARTI: Okay, so we've seen obesity rise in all age groups in the United States.
So help me understand a little bit more about first of all, what it is about obesity that that leads it to be a major risk factor for gastrointestinal cancers. And actually, Dr. Ng, I'm going to start with you about that. How does it trigger the development of a cancer?
NG: We are still trying to work through that, but we do know that a state of obesity does lead to inflammation in the body, and we do know that inflammation can promote cancer.
We also know that it can lead to things like insulin resistance, and the insulin signaling pathway is very important in the pathogenesis of many of these cancers. I think what's different here, is that we do think exposure in early life to a risk factor is important for the subsequent risk of cancer in later adulthood.
And as you know, childhood and adolescent obesity has increased dramatically, as well. So that might be why it's happening to younger people.
Part II
CHAKRABARTI: And Dr. Rebbeck, I understand that you're also looking at sort of genetic factors here. Do the two meet in any way, in terms of obesity? And then perhaps, I don't know, triggering the release of something that was previously embedded in a person's genes?
REBBECK: Yeah, I think that's exactly right. Over this short period of time, the genetic profiles of people are not changing. So we're not suggesting that genetics are changing to cause these new incidences of early onset cancer, but that whatever is underlying your genome and makes you susceptible to cancer is being triggered earlier.
So maybe people who have had a genetic susceptibility and would have been diagnosed at age 60 are now being diagnosed at age 40, because of some of these environmental exposures or lifestyle exposures that have changed very rapidly.
CHAKRABARTI: Are we seeing similar rates of growth in early onset cancers in other countries?
REBBECK: Yes, this is a phenomenon that's happened worldwide, which makes it very interesting. It's not something that's just occurring in the United States or places with, you know, certain dietary lifestyle patterns, but it's really happening everywhere. We don't have great data for every part of the world, and there are also varying patterns.
So it also seems that some countries, like Japan, for example, which is high income country. Good health care, all those sorts of features, but has less of a Western diet. Western lifestyle influence is not having as strong an increase in some of these cancers. So that's all very ecological and not necessarily proving anything, but it certainly is giving us a sense of what kinds of exposures, what kinds of lifestyle factors may be going on around the world.
CHAKRABARTI: Dr. Ng, did you want to add to that?
NG: Yes, we are seeing differences in dietary patterns, where we see much more of a Western pattern diet, increase in processed foods, red meats, sugars. And that seems --
CHAKRABARTI: In other countries? Is that what you're saying?
NG: Well, so in these higher socioeconomic status countries, where this Western lifestyle is predominant.
That's why we suspect that may be linked to why the rates of these early onset cancers are rising most dramatically in those regions of the world.
CHAKRABARTI: I see. Okay. So, Dr. Rebbeck, let's, we can just step away from the gastrointestinal cancers for a moment. Are there any other theories about the other forms of cancer?
REBBECK: I think that when you move away from factors that are clearly linked to diet and lifestyle, it becomes much more difficult. The risk factors for cancer include smoking and alcohol consumption and some of those kinds of other factors and those are very clear.
When we get to something like environmental toxins, environmental chemicals and things like that. That's much harder to study. It's much harder to understand. As Kimmie was saying, it's very important to have, to understand early lifetime exposures. And that's really hard to do. If I ask you, "Were you exposed to pesticides or chemicals as a child?"
You probably can't answer that question very well. And that's the kind of data that we would need to really understand that question. For some of these other cancers, where the risk factors are less clear, we have a very hard time understanding what their causes may be. And so we're really early in our understanding of these causative issues.
CHAKRABARTI: Yeah, this is such a mystery, right? Because first of all, there's the challenge in teasing apart causation, because it could be multimodal, right? And then as you're saying, a lot of it is just nearly impossible to measure. Quite frankly, we're swimming in a sea of chemicals all the time. But Dr. Ng, let me turn back to you on something.
Are we also seeing a sort of a differential rise in rates when it comes to people of different socioeconomic status, or race is always a question when it comes to things like cancer? Or is it like across the board an equal increase?
NG: So actually, the latest data suggests that this rise is being seen in every racial and ethnic group in the United States.
But the rate of rise seems to be steepest in non-Hispanic whites, such that some of the racial disparities that we're very well aware of when we think about incidents and mortality of this disease is narrowing. And we don't understand why it is that the rate of rise does seem to be highest in that population.
CHAKRABARTI: Okay. What I'm about to ask probably doesn't, or say, doesn't apply to the colorectal cancers that we talked about in the early in the show, because screening does happen now at 45 and later, but we did also actually speak to another physician who said maybe for some of the other cancers, part of the reason for the rise in the rate might be what we call cancer.
Okay, and I'm going to emphasize the physician told us this is a partial explanation. Because we spoke with Dr. Laura Esserman. She's a surgical oncologist and director of the multidisciplinary breast cancer program at the University of California, San Francisco. And she says some of these diagnoses of what we call cancer don't actually pose much of a long-term health risk.
Some of them. But the label cancer can compel doctors and patients to leap to aggressive treatments like chemotherapy or surgery. So perhaps for conditions that rarely lead to harmful or malignant disease, Dr. Esserman says we should maybe stop calling them cancer. And she gave us a specific example of ductal carcinoma in situ or DCIS.
LAURA ESSERMAN: The more you screen, the more you're going to find. And some of the things that you find are not necessarily disease that's going to kill people. And so I think you have to ask yourself, we treat everybody with DCIS as if it's a Stage 1 cancer. At 10 years, the survival rate's 97%.
So by waiting, you're not causing harm. And if you follow people carefully and you don't operate on them from the beginning, the majority of people don't ever need anything. Why are we calling that cancer? That's not the same thing. So that's why taking the word out, I think, is super helpful. It's really important for not overreacting and not overdoing it.
And again, nobody's meaning to do any additional harm, but it's hard when you hear that word.
CHAKRABARTI: Dr. Rebbeck, I did want to raise this issue because there are some forms of cancer that in the recent past, we've seen recommendations for screening change to have the years be further apart.
For example, prostate cancer is a good example. What do you think of Dr. Esserman's Idea that some of what we're seeing may be because we're calling things cancer at an earlier stage that she says may not necessarily end up being truly malignant.
REBBECK: Her point is taken and I think many people in the field are considering some cancers like breast, early breast cancers, prostate cancer, thyroid cancers that often don't lead to mortality as being thought of as something different than the kind of cancer that's going to kill you and needs treatment. And so she's correct in thinking about that. The problem is we don't have a very good handle on which of these cancers are going to go on to be lethal and which ones aren't.
And I use the example of prostate cancer. There are tigers and kittens. The tigers in prostate cancer will kill you and they're relatively rare. But if you have one of those, you certainly want to treat it and be aggressive to improve the chances of survival.
But most prostate cancers are diagnosed at a relatively early indolent stage and they'll never go on to kill you. And you want to find, be able to find those and not treat them. Because men who undergo prostate cancer treatments can have all sorts of side effects particularly in the early onset setting where men that are fairly young will have a long life ahead of them and they don't want to have the impotence and incontinence and some of the other treatment side effects if these cancers aren't going to kill them.
So those points are actually very well taken. We just don't yet really know who's going to be a good actor, who's going to be a bad actor and how to manage those when the diagnosis occurs.
CHAKRABARTI: Yeah. Dr. Ng, as you said earlier, I acknowledge that the patients you see often have Stage 3 or 4 cancer, so there's no doubt that they're serious. But I just wanted to quickly hear from you about looking at the broader spectrum of the stages of cancer and what we should call what, when?
NG: Yeah, I know. And I agree that those points are really well taken. But I do emphasize that we need research to better understand how do we predict which tumors are not going to kill you and which ones are. And in that way, we can then either escalate or deescalate treatment according to that individual's profile.
So we're not quite there yet, but we need to get there. It seems as if there are so many unknowns still. And maybe we expect too much out of medicine and science sometimes to think that we're going to like just a couple of studies in a couple of years and we'll have all the questions answered. That is not the case here.
But I'm thinking back to something that Michelle, the caller from Vancouver, Washington, said that she had the thyroid cancer at a young age. And when she went to seek a physician's help, they had to ask her all ranges of questions, including, had she gone to Chernobyl? What does that tell us about how little we know even at the beginning stages of trying to seek a diagnosis?
NG: I think it tells us a lot. Not only do we have to look at known risk factors that have been linked to these cancers, no matter what age you are, but we also have to think completely outside the box and investigate recent changes, recent new chemicals, recent new toxins, and then figure out how they are leading to cancer.
And some of these are affecting us starting in early life. How do we assess that? And so we're trying to it administer questionnaires, but as Tim said, the recall is not always perfect. So how are we going to study these early life exposures and how they actually lead to cancer?
Part III
CHAKRABARTI: We heard a lot from listeners. So this is Jennifer. She told us that she was diagnosed with cancer four years ago at the age of 44 with acute myeloid leukemia. Two years later, she was also diagnosed with breast cancer. And now, even though both are under control, the diseases are always in the back of her mind and it's changed her approach to life.
JENNIFER: How it's changed my life is that I, working much harder at living in the moment and not putting things off. None of us know how long we have how much life we have left. But when you're faced with the prognosis that could be life altering and life ending, you go ahead and do some of the things that you've wanted to do and enjoy life a bit more.
CHAKRABARTI: We're going to hear from more listeners in a bit, but I want to take a moment to thank everyone for sharing their stories with us. Before we get to what can we do, I just want to go back to one thing, which both of you emphasize is quite important, the obesity connection and the, I guess, diet connection here when we talk about highly processed foods or changes in diet, Dr. Ng, can you tell us more specifically what kinds of foods or what does highly processed mean in terms of the rate of these cancer increases?
NG: Yeah. So highly processed means, they're not natural. They're not growing from nature; they're not fruits and vegetables.
If they have these substances that preserve them for a long time, and we don't yet know how those things may lead to an increased risk of cancer, but we highly suspect that perhaps they're shaping our microbiomes. And our microbiome, we know has a lot to do with many different chronic diseases, and it may actually be contributing to why these cancers are rising in younger people.
Okay. So highly processed than what you just described sounds like everything in a grocery store except for fresh produce, meats, fresh meats, things like that. It's the majority of the American food supply almost.
NG: Yes.
CHAKRABARTI: And so what does, that seems like it puts people in a challenging place.
NG: It does. And I think this speaks to the importance of public health messaging and efforts to really try and educate people starting in childhood and adolescence about what a healthier diet may be. And we do think it's one that's more healthy proteins, and fruits and vegetables rather than some of these highly processed sugars and meats to follow throughout life, to hopefully decrease the risk later in adulthood.
CHAKRABARTI: Okay, then regarding the microbiome, what can people actively do to protect and keep their microbiome healthy? So a lot of the diet and lifestyle factors we recommend to try and reduce the risk of all cancer types probably make you have a healthier microbiome. And this includes maintaining a healthy body weight, exercising as much as you can, following these healthier diets, not drinking, not smoking.
CHAKRABARTI: People are going to ask about probiotics.
NG: We don't yet know what the good organisms in the healthy microbiome are. So right now, at least for cancer treatment or prevention, we don't routinely recommend probiotics until we get more information and research.
CHAKRABARTI: Okay. I also now, thank you for that, because we're talking about something that I think people do need just really elemental advice on what they can do.
And there's no silver bullet here yet. But almost as cancer prevention 101 is what we want to get out of this hour, as well. So another factor that both of you discussed was the other environmental factors, including potential chemical exposure and how that is hard to measure.
So we spoke to someone about that. Because we're talking about chemicals like the PFAS chemicals, are also called forever chemicals. They are found in a lot of goods, including some textiles, even dental floss. There's also a class of chemicals known as endocrine disruptors, found in a lot of personal care products.
So we reached out to Dr. Julia Brody. She's executive director and senior scientist at the Silent Spring Institute. They research the environmental causes of breast cancer, the most common, or one of the most common early onset cancers. Interestingly, there are more than 12,000 cases diagnosed each year in the United States.
JULIA BRODY: There is a lot of science out there now about environmental chemicals and cancers. One of the things that my own research has been focused on is telling people about chemicals in their bodies. And we developed a lot of knowledge related to how you can reduce your exposures. What will we say are some of the top priorities?
I think not using pesticides in your home is a good starting place. Avoiding fragrance products, many of which contain endocrine disruptors. Those are some easy starting places.
CHAKRABARTI: Dr. Rebbeck, you said earlier that the chemical connection is quite hard to pinpoint as causal, right? Because, people have difficult time remembering their exposure, may not even know it, right?
But can we say definitively at all that we should be looking to environmental chemical exposures as a potential cause of these earlier cancers?
REBBECK: I think this is an area of research that needs to be done. As we've said, it's not easy to figure out what these the causation mechanism is for these chemicals and cancer.
And most of the data that we have from large human studies, large epidemiological studies don't give us a lot of evidence that there is a large effect, a major effect of these chemicals. That's not to say there isn't an effect there, it's just hard for us to detect it in human studies.
And we believe that animal studies are probably not adequate to really understand what's going on in people. So I think that this is the classic, we need more research, and we need clever ways of doing research because trying to assess people's memories of what they're exposed to is not ever really going to work.
At least we haven't found a way to make that work. So I would also say that these chemicals are really important. I agree with Dr. Brody that there's not, if you can avoid these chemicals, if you can do something to eliminate them from your life, that's fine. But I would also point out that the major risk factors still are things like smoking, alcohol consumptions, diet, and those are the things that are probably more impactful in lowering your risk, given the scientific data we have right now.
CHAKRABARTI: It's so interesting when very frequently part of the answer is more research. And I really, I do take that point quite strongly. Because all of science, medicine, is almost like you're operating in a dark, you're working in a dark room and you try to understand as much as you can about that dark room, but you're limited to where you shine your flashlight.
There's much more to be seen, which is why we need that more research, but it sounds like we're still only illuminating a small corner of that room, Dr. Ng. So I just, with that in mind, I wanted to ask you what you think about the chemicals in our environment question.
NG: Yes, I think it's very reasonable to study them.
We, again, just still don't know a lot right now. And we are trying to tackle this from multiple angles. We're trying to do these epidemiologic studies, but it's hard. We are trying to study them in mouse models because you can more easily control this environment. And you can expose these mice early in life to these chemicals and see what happens.
Do they develop cancer? Do they develop cancer at a younger age? So we're experimenting with all these things. But again, I think the ideal study is to start studying people from in utero, through infancy, through childhood, through adolescence, collect all this information on their lifestyle, collect specimens and then follow them through time.
But that study is very hard to do. Costly and probably takes too long. So we need other ways.
CHAKRABARTI: Maybe one other way, again, just another little piece of the puzzle here is trying to leverage what we know about cancers in older people. I do wonder about that. Because we spoke with Dr. Peter Campbell. He's a professor of cancer epidemiology at Albert Einstein College of Medicine.
And of course, he too also acknowledged there's so much that we don't know about early onset cancers. But he also told us there could be lessons in cancer prevention that we learn from later onset cancers.
PETER CAMPBELL: Earlier and later onset colon cancer and look a lot alike under a microscope and molecularly, so it makes sense that the risk factors are probably going to overlap, too. So we feel comfortable saying, avoid smoking, avoid obesity, be more physically active because it seems safe to suggest that those are probably going to be similar.
CHAKRABARTI: Dr. Campbell also told us that people under the age of 50 need to be aware of potential symptoms and see a doctor if they're having any kind of abdominal pain, blood in the stool, unintentional weight loss, that kind of thing. Dr. Rebbeck, let me first hear from you on this.
It's interesting to me that he said that early and later colorectal cancer, at least, they look very similar under a microscope and molecularly. What's significant about that?
REBBECK: I think first of all, it's telling us that there are the causes, the ideology, the carcinogenesis pathways may be quite similar.
But I would also say that's not necessarily true, or we don't know if that's true for all of these cancers. There's been relatively limited studies of early onset pancreatic cancer, for example, or gallbladder cancer in young and old diagnosed individuals. And so I think there's still a lot that we can learn from the molecular or the histological characterization of these tumors to understand whether there are differences.
And not only whether the causes are different, but whether the tumors are different enough that we might want to manage or treat them differently. And whether that gives us signals that we can use to screen or detect these cancers early. So I think this is an important area of research we still can leverage to better address the early onset problem.
CHAKRABARTI: Alright, let's hear from a couple of more listeners who shared their stories with us. First, this is Shirley from Albuquerque, New Mexico. Her son was diagnosed with Stage 4 mantle cell lymphoma, and more than a decade later, fortunately, he is in remission.
SHIRLEY: I'll tell you what helped my son, who got cancer at 40, the clinical trials.
Back east, in New York City, helped my son. Thank heavens for clinical trials.
CHAKRABARTI: There's also Dusty, who shared this story with us. She was diagnosed with Stage 2B breast cancer at age 40. Had no family history of the disease. That seems to be something common amongst these early onset cancers. That form of cancer had never shown up previously in the patient's family.
Dusty ended up having a full right-side mastectomy.
DUSTY: It also showed me just how vital early detection is. They told me that one in eight women have breast cancer and it just, we're fortunate that we have really good health insurance. So it wasn't even a question to just go in and have it done. But I know so many women can't afford that luxury, and it just breaks my heart.
CHAKRABARTI: Okay, Dr. Ng, as you well know, we cannot have a conversation about American health care without talking about cost and insurance. Dusty there acknowledged that she has good health insurance, so fortunately she could get the screening. But we're talking about people who are unusually young when it comes to what an insurance company might see as a target demographic to approve screenings.
And so I wonder how much of a challenge that may be, as we go forward thinking about what to do here. Because if the guideline is for colorectal cancer, for example, screen at 45 and after. But we're looking at people in their 30s or possibly even 20s. It doesn't seem to me that an insurance company would find that to be adequate evidence to approve screenings when maybe that's what we need.
NG: That's right. According to the Affordable Care Act, the health care companies are required to cover screening according to the guidelines. So anyone age 45 at average risk will have that covered by insurance. Still, there are some barriers and issues to work out. But this is why it's important to actually ask your family about your family history.
Because if there is, for example, a first degree relative who has had colorectal cancer or an advanced polyp at a young age, you may be eligible to get screening earlier and then insurance companies may cover that. But for the vast majority of the 20-year-olds and 30-year-olds, this is why we need more research about the causes of underlying young onset cancer.
If we know the causes and we can identify those who are at high risk and target that population for earlier screening.
CHAKRABARTI: We got an email today, actually, from another physician, Max Tilson, who's the vice president of the Massachusetts GI Association, and he told us that one concern that he has is that there are forms of screening, particularly for colorectal cancers, because colonoscopies are not fun for anybody, but you might get more people to come in and do it if they can have greater sedation, but he knows for a fact that big insurers won't cover that increased amount of sedation.
So that's another hurdle to have to clear here. But Dr. Rebbeck, I wonder, in terms of developments in medicine, are there people working on forms of screening that are less invasive, for example? Leaning on your experience as a geneticist as well, are there ways to just learn more from blood samples?
I don't know, am I groping around here in the dark? But go ahead, yeah.
REBBECK: Yeah, you're not groping at all. In fact, the one of the most promising avenues for early detection right now are multi-cancer, early detection liquid biopsies that are being developed. And the advantage of these are that they're using molecular signatures that are floating around in the blood to identify the presence of cancer very early.
They're not really ready for prime time, but in the coming years, they're going to completely change the landscape of cancer early detection and screening. They can be ideally implemented outside of the health care system. So you could go to a big box store and have you have this, one of these tests done.
You could do it from home and they will either supplement existing screening technologies or for the many of those that we're talking about today where there is no screening currently, they will allow us to screen for multiple cancers and they ideally will be cheap, accessible, and we really have a lot of promise in that area coming up.
This program aired on September 15, 2023.

