Advertisement
Your brain on menopause
Resume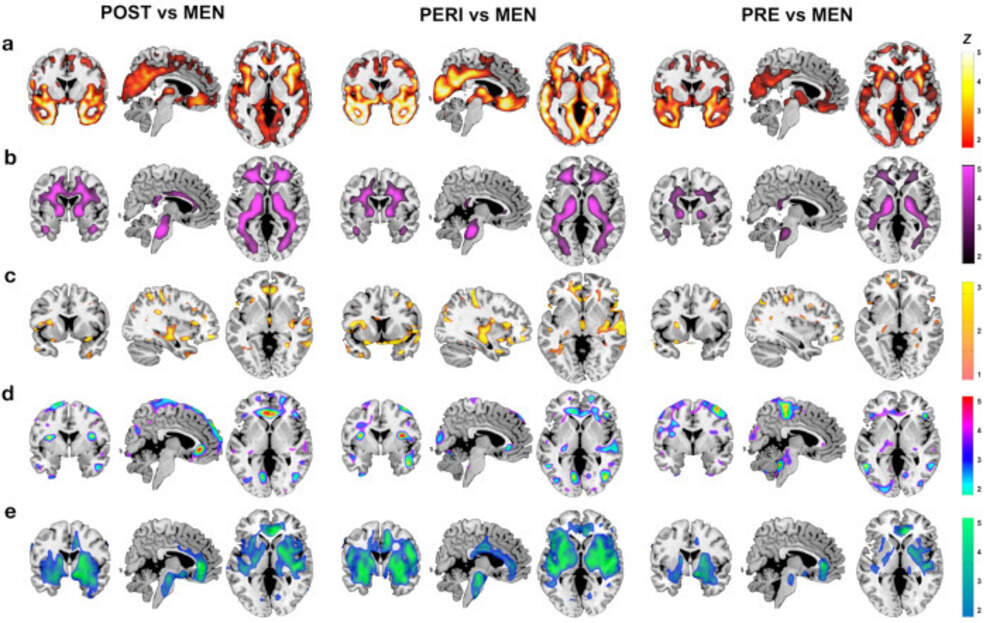
Hot flashes. Brain fog. Sleep problems.
Millions of women go through menopause each year.
But what’s happening in the brain during this life transition?
Today, On Point: The new science on menopause.
Guests
Lisa Mosconi, neuroscientist and director of the Women’s Brain Initiative at Weill Cornell Medicine. Author of the forthcoming book “The Menopause Brain: New Science Empowers Women to Navigate the Pivotal Transition with Knowledge and Confidence." Her previous books are “The XX Brain” and “Brain Food."
Also Featured
Dr. Jan Shifren, reproductive endocrinologist and OB/GYN. Director of Massachusetts General Hospital Midlife Women’s Center. Professor of Obstetrics, Gynecology and Reproductive Biology at Harvard Medical School.
Transcript
Part I
MEGHNA CHAKRABARTI: Menopause. Millions of women go through it every year.
(LISTENER MONTAGE)
LILA ANNA: I was sobbing on the phone in rush hour traffic. I hadn't been sleeping, I was having these weird mood swings. And I called my OB/GYN. He listened and basically said, “I'm not going to give you a pill for this.”
ANDREA HARDY: Most of my friends have either gone through this transition or currently going through it and they don't want to talk about it.
ANGELA EVERITT: I had to ask the questions. I had to do the research. This aspect of my health feels completely ignored in the medical establishment.
SARAH VINAL: My mom never talked about it. Primary care never set me up for this. I feel like even society hasn’t prepared me for this.
MARA MARTINEZ: And what I am going through. I feel absolutely invisible.
CHAKRABARTI: On Point listeners Lila Anna in Columbia, South Carolina; Andrea Hardy in Portland, Oregon; Angela Everitt in Arlington, Virginia; Sarah Vinal in Portland, Oregon; and Mara Martinez in Indian Head Park, Illinois.
Today we are going to talk about menopause, specifically what the latest science shows us about how it affects women's brains.
Lisa Mosconi joins us. She's a neuroscientist and director of the Women's Brain Initiative at Weill Cornell Medicine in New York City. And she's also author of the forthcoming book, “The Menopause Brain: New Science Empowers Women to Navigate the Pivotal Transition with Knowledge and Confidence." Lisa, welcome to On Point.
LISA MOSCONI: Hello, happy to be here.
CHAKRABARTI: We have a lot of listeners, of course most of them women listeners, who responded very positively to the fact that we were going to have this conversation.
MOSCONI: Of course. But I wanted to start with how you became interested in menopause and the brain, because obviously you've written a lot about the female brain before.
At least, a couple of other books, “The XX Brain." And you've also written a book called “Brain Food." But can you tell us the story of how you became interested in focusing on menopause as a neuroscientist?
MOSCONI: Yes. And thank you for asking. It is an interesting story because I really, I would never have thought that one day I would be here on NPR talking about menopause. I am a brain scientist by training, and I have a dual PhD in neuroscience and nuclear medicine, which is a branch of radiology. So I do a lot of brain imaging for my line of work, and I actually specialize in the prevention of Alzheimer's disease and support of cognitive aging.
So dementia prevention really has been the major focus of my work for the past 20 years, since I was very young. And that's because I have a family history of Alzheimer's disease that affects the women in my family. And it turns out I'm not the only one. Currently, almost two thirds of all Alzheimer's patients are women.
And this gap and this higher prevalence was dismissed for many years in medicine by people saying women live longer than men.
CHAKRABARTI: I was just going to say that. I thought that was the presumption, right?
MOSCONI: Yes. I've been getting this pushback, pretty much my entire life at this point, but it really came with this question.
And I was like, "Does it matter if you're a woman or if you're a man in terms of Alzheimer's risk?" And everybody would tell me, "No, really, the point is that Alzheimer's is a disease of old age, and women live longer than men, therefore, at some point, more women than men will have Alzheimer's disease." And that never made sense to me, in part, because women don't live that much longer than men, maybe a couple of years longer than men, but not like a decade longer.
But then mostly my PhD work was really focused on showing that Alzheimer's disease is not a disease of old age. It's actually a disease of midlife with symptoms that start in old age. So in other words, Alzheimer's starts with negative changes in the brain, years, if not decades before clinical symptoms emerge.
So that changed our entire question to, all right, so if more women than men have Alzheimer's disease, and Alzheimer's is a disease of midlife, what happens to women and not to men in midlife that could potentially increase the risk of developing Alzheimer's? And by doing a lot of different studies and brain imaging evaluations, running a lot of different experiments, we found out that menopause seems to be a potential trigger for Alzheimer's disease in women's brains already in midlife.
So that's how I ended up studying menopause, really, which is now a huge focus of our research.
CHAKRABARTI: So I have a couple of follow up scientific questions to that.
MOSCONI: I'm sure, yes.
CHAKRABARTI: But also, I think if I remember correctly, there was essentially a kind of a eureka moment around --
MOSCONI: Yeah.
CHAKRABARTI: Can you tell us that story?
MOSCONI: Oh, yes.
Yes, of course. This is interesting, because we were, so we've been working with individuals who are in their 40s and 50s and 60s, because we're able to detect the earliest possible signs of Alzheimer's disease in the brain, but using brain scans, already at that age. And so when we compared women's brains to men's brains, we would find that women's brains were more Alzheimer's than men's brains already in midlife. And the question is like, why? Is it just female sex? Is it just being born with two X chromosomes and ovaries? Or is there something more? And we started looking at everything that could explain this difference.
We started with genetics, of course, and family history and that helped a little bit, but not quite to explain these differences. And then we looked at medical risks, diabetes, thyroid disease and insulin resistance and cardiovascular risk factors, and that didn't quite help. And then one day, my students were doing cognitive testing on one of our participants.
A woman, of course, who was having a hard time, and she was having a hard time just focusing and performing the cognitive tests. And she said, I really need a break, and can you please open the window?
CHAKRABARTI: Oh dear.
MOSCONI: And my students were like," What? Sure, yeah, by all means, take a break." We usually offer water.
"Why the window?"
And she said, "Because I'm having hot flashes, I can't think straight." And they were all like, "You're having what?" And then eventually she just couldn't do the testing and they ran back to me and said, "This lady unfortunately had to leave, we're going to reschedule, but we were very worried.
She said that she needed to open the window, she needed air, she was having hot flashes?"
They didn't know what that meant.
CHAKRABARTI: (LAUGHS) Oh dear God.
MOSCONI: They had no idea. Because we never really talked about menopause before. And then I say," Oh, hot flashes." She was having, I explained, "It's a sign of menopause." And even though she's young, she was young, she was in her 40s and a lot of people mistake, in quotes, menopause for something that happens to you when you're old, right?
And 40 is not old by any definition. So they were really surprised. And then we went, then I called the OB/GYN department, and I said, "We really need to start looking at menopause." And so we went back, and we asked every single person in the study about their menopausal status and then we were able to show the differences.
So when you take a group, at least in our hands, when we're looking at women who are premenopausal, they have a regular menstrual cycle, and we compare them with a group of men who are matched by age, exactly the same age, then we didn't find any differences in their brains. But when the women were perimenopausal, so when they started having an irregular menstrual cycle and the hot flashes, the night sweats, and those symptoms, then we started seeing an increase in the red flags for Alzheimer's disease in their brains as compared to men who were exactly the same age.
And when the women were actually at the postmenopausal stage, then we really saw a clear-cut difference in terms of Alzheimer's risk.
CHAKRABARTI: Okay.
MOSCONI: And that was quite, whoa.
CHAKRABARTI: Yeah. Okay. So I'm going to come back to, we'll speak in more detail about your research regarding Alzheimer's and menopause because I know a lot of people are probably like, what?
But I actually just want to take a moment to be sure that we all have a collective, accurate understanding of exactly what menopause is. So we actually reached out to Dr. Jan Shifren. She's a reproductive endocrinologist and OB/GYN, and she also directs the Midlife Women's Center at Massachusetts General Hospital, and she offered us a quick menopause 101.
DR. JAN SHIFREN: Menopause is really when the ovaries have come to the end of their reproductive life. The ovaries have two major parts, one of which is called the granulosis cells, the kind of structures in the ovary that are responsible for making estrogen throughout reproductive life. With menopause, you can actually look at an ovary on an ultrasound and see that these follicles have disappeared.
We think that this is basically genetically programmed cell death of these important cells in the ovary that again are responsible for eggs and for most of the reproductive hormone.
CHAKRABARTI: And Dr. Shifren says two of the most important hormones, estrogen and progesterone.
SHIFREN: Typically, the ovary will make estrogen for most of the, let's say, 28-day menstrual cycle.
And then the ovary will also make a second hormone called progesterone for the second half of the menstrual cycle. The major goal of both of those hormones for cycling women is to basically prepare the lining of the uterus, what we call the endometrium, for pregnancy. With menopause, the ovary is no longer doing that beautiful cycle with the estrogen and then estrogen and progesterone.
And so basically the hormones, estrogen and progesterone are very low when a woman is menopausal. There's still other places in a postmenopausal woman's body where she does make some estrogen, but not nearly the same amount she made when she was cycling regularly.
CHAKRABARTI: And Dr. Shifren says it's that drop in estrogen that can cause things like bone loss, hot flashes, trouble sleeping. So that's just a little refresher from Dr. Shifrin. Again, she's a reproductive endocrinologist and OB/GYN. We're going to hear more from her a little bit later in the show, for her answer to the question that I think most of my fellow ladies listening right now want to know, which is should you or shouldn't you take hormone replacement therapy?
But that's going to come a little later in the hour. Now we've got just about 30 seconds before our first break, Lisa, I just quickly want to know if, so you want to reassure people that the first part of your book is all about you are not imagining this. This is actually happening to your body, right?
MOSCONI: Yes, absolutely. Menopause is a neurologically active state. It changes your brain as surely as it changes your ovaries.
CHAKRABARTI: Okay, so we're going to talk about what those brain changes are when we come back from this break.
Part II
CHAKRABARTI: We did hear from many of you who are experiencing menopause right now, and you shared what some of your symptoms are.
So let's listen.
(LISTENER MONTAGE)
ANDREA HARDY: It hit me like a freight train.
MELISSA PAUSER: By age 45, I was having hot flashes.
SARAH VINAL: I developed depression and severe anxiety.
KATE NOTMAN: Barely slept for months on end.
KRIS GASTON: I would be driving somewhere and suddenly wouldn't remember where I was going.
BRIGETTE DINEEN: 10 to 15 really bad, sweaty hot flashes a day.
ANDREA HARDY: Bloating, breast tenderness, noticed about five pounds around my middle. Urinary incontinence, which has not been fun.
BRIGETTE DINEEN: These things called “doom drops” when you're just going about your day, minding your business and all of a sudden just this terrible feeling comes out of nowhere and makes you feel like garbage.
PAMELA: I call it “wet cat.” “Wet cat” is a feeling of being out in the rain with no raincoat.
CHAKRABARTI: That was Andrea Hardy in Portland, Oregon; Melissa Pauser in Watsonville, California; Sarah Vinal in Portland, Oregon; Kate Notman in Stow, Massachusetts; Kris Gaston in New Kent, Virginia; Brigette Dineen in Lakewood, Ohio; and Pamela in Maine.
Okay. So Lisa, the body is this like masterful homeostatic machine. So can we say definitively whether is it changes in the brain that cause menopause or is it changes in the reproductive system that that produce the brain impacts that those women were describing? What's actually going on that you can see through your research so far?
MOSCONI: And that's such a good question and such an important question. Because we just heard a lot of women just don't know what hit them during menopause and a lot of physicians as well. A lot of doctors do not recognize the symptoms as something related to menopause. And I think what's missing here is that, as a society, we basically focus on half of what menopause is all about.
And most people realize that menopause is associated with something changing in the function of the ovaries. The ovaries running out of follicles, your menstrual cycle ending, the end of fertility. But we have completely lost track of the fact that menopause is defined as a neurological, as a neuroendocrine transition state, which means that your brain, your neurological system, is changing together with your endocrine system, with your ovaries and your hormones.
So this transition, in fact, impacts the brain just as much as it impacts the ovaries.
CHAKRABARTI: But why? Yeah, but why? Why is it that sort of a draw? Let's say a programmed cell death that Dr. Shifren talked about earlier.
CHAKRABARTI: ... Why is it that drop in estrogen would have such an impact on the brain.
I guess, does that imply that estrogen is an important hormone for the brain at any time for a woman?
MOSCONI: Yes. So estrogen has been mislabeled a sex hormone in the 1930s by scientists who were studying reproduction and they found estrogen. And linked the function of estrogen with fertility and having kids and having babies.
But it wasn't until much later, in the 1990s, the scientists realized that the same exact hormone plays a hugely important function for our brain health. So sex hormones are actually neuroprotective hormones that literally shield your brain from harm.
CHAKRABARTI: How? So estrogen in particular has been called, is referred to by scientists as the master regulator of women's brain health.
MOSCONI: And that's because we are born with the neuroendocrine system that connects our brains with our ovaries. And this system is activated during puberty, is over activated during pregnancy, every time a woman is pregnant, and then it's turned off with menopause. And the way that the ovaries and the brain communicate is by using these hormones like estrogen, progesterone, which are made by the ovaries, but also by the brain.
And then the brain releases different hormones called FSH and LH that go down to the ovaries and say, "Okay, we need more estrogen here." So it's really a feedback loop that ensures that the brain is in communication with the ovaries every minute of our lives as women. So you need to think about it this way. Every time your ovaries cycle, your brain goes through a micro cycle, where all the things that are powered by estrogen increase when your estrogen levels are high and decrease when your estrogen levels are low.
And these things are like neuroprotection, immunity inside the brain, the amount of dendrite, the amount of little branches that your neurons make, increase and decrease during different parts of the menstrual cycle in response to estrogen levels. Brain energy level changes in response to estrogen stimulation.
In some ways, estrogen is to your brain what fuel is to a car.
CHAKRABARTI: Wow.
MOSCONI: It keeps it running. Yes.
CHAKRABARTI: Okay, so if I can. Okay. So you said that the number of dendrites actually grows?
MOSCONI: Yes, we can see it. We can see it with imaging. We can see it in vitro. Yes, it's really pretty.
CHAKRABARTI: So does that mean --
MOSCONI: To me.
CHAKRABARTI: No, it's beautiful.
It sounds beautiful. I'm trying not to be overly simplistic about this, but I can't help it. What is the impact of the increase in number of dendrites in the brain? Does it make the brain more capable? I don't know how to put it.
MOSCONI: Capable, is more a psychologist may use this term.
From a raw biological perspective, it makes the brain more connected. It gives you a little bit more resilience and it doesn't really translate necessarily into behavior. Although we do know that for some women, there are changes in brain fog, in focus and concentration and mood already during the menstrual cycle.
CHAKRABARTI: Yeah.
MOSCONI: Many women experience PMS.
CHAKRABARTI: Yeah. Again, it seems, again, we can't, I totally take your point about that we can't draw a straight line between what's physically happening and psychological experiences, but it almost seems a little ironic that when you have an increase in the number of dendrites, one of the symptoms people often feel is, women often feel, is brain fog.
One would think that. --
MOSCONI: No, the opposite. So when the dendrites --
CHAKRABARTI: It's a decrease.
MOSCONI: Yes. Yeah. So that's when you feel more energized around ovulation. Usually you feel more on point, if you will, you feel more focused, you have better energy, better mood, more libido in some ways. And then towards the end of the menstrual cycle with estrogen withdrawals and progesterone is there, once you prepare for the menstrual cycle, these hormones withdraw and so do your dendrites.
CHAKRABARTI: I see.
MOSCONI: And then you may feel a little bit more tired, and these are very subtle changes, to be clear. These are microscopic changes, but there are changes that are important in terms of cellular activity, cellular energy, cellular aging, very important. If I may add, because I don't want anybody to be scared, menopause does not cause Alzheimer's disease.
CHAKRABARTI: I was going to ask you about that. Yeah. Tell me more, because when we started the show, I was like, oh, people are going to be worried that if they go through menopause, yeah, that Alzheimer's is inevitable.
But obviously that's not the case.
MOSCONI: No, it's totally not the case. So about 20% of women develop Alzheimer's disease in their lifetime, which is way too many for my taste, but it also, since every woman develops menopause at some point or the other in their lives, it also tells us that there's more, there are many other factors that interact and intervene, and that Alzheimer's disease is a very complex disorder.
What we understand about menopause is then it's a transition state. It's a state in which your brain is left a little bit more vulnerable because we're losing the superpowers of estrogen and progesterone that keep your brain energized and active and youthful, in quotes, from a cellular perspective.
So your brain is a little bit more vulnerable, which means that some medical risks may then become actual medical symptoms as women go through menopause. For instance, if a woman has a predisposition to major depression or to clinical depression, chances are that she may experience depressive symptoms for the first time in her life during menopause.
If a woman has a predisposition to an autoimmune disorder like multiple sclerosis, chances are that the first signs of multiple sclerosis in the brain will become visible around the menopause transition. And the same seems to be happening for Alzheimer's disease. If a woman has a predisposition to Alzheimer's disease, then menopause is when we start seeing the red flags for the disease, but it does not mean obviously that all women will develop Alzheimer's disease.
That would be an overstatement. We're just saying that estrogen is a neuroprotective hormone and it's been studied, studying, in relationship with Alzheimer's disease risk, and there seems to be a connection that needs to be explored further, for sure, and that will also inform treatment options and preventative options, but absolutely do not be scared.
Menopause does not cause Alzheimer's disease. What it can do is being evaluated as a female specific risk factor for Alzheimer's.
CHAKRABARTI: Okay. Thank you for that clarification.
MOSCONI: Does that make sense?
CHAKRABARTI: Totally.
MOSCONI: Okay.
CHAKRABARTI: Yeah, absolutely. It sounds, it makes perfect sense. Because there are other stages in life where people become vulnerable to other things.
MOSCONI: Yes. Puberty, pregnancy. Yeah, exactly. I think it's important to see this continuum, that if you had anxiety attacks during puberty, which is very common for women, and you had anxiety again during pregnancy, chances are you will have Alzheimer's, sorry anxiety during the transition to menopause.
There's a continuum because this system is activated and deactivated at different turning points in a reproductive life, but it's the same system.
CHAKRABARTI: But it doesn't have to be a permanent state once you're in menopause, if you say using the anxiety example.
MOSCONI: Absolutely. Typically for most women the symptoms that are triggered by the menopause transition go away within sometimes four to six years after the final menstrual period.
For some women, just two years. For some women, it takes a lot longer. And for some women, unfortunately, the symptoms do not go away. So I think it's really important to appreciate the menopause is not a one size fits all situation, although it's been portrayed as such medicine, unfortunately, at this point, but rather it comes with a range of possible symptoms and combinations.
Symptoms and severity of symptom that really has no framework currently, but needs to be formalized because it's so important to acknowledge that like with pregnancy, some women have no mood issues with pregnancy, some women have the baby blues, some women experience postpartum depression, and a few women experience postpartum psychosis which is very severe.
And there's evidence that a similar range of symptomatology may be present with menopause. It really has not been studied, but should be, because that validates women experiences and gives them the wording and the vocabulary to not only describe their symptoms to their doctors, but also to seek treatment that is appropriate for the severity of their symptoms.
And we do that for brain fog, for example, and cognitive changes and memory decline. A lot of our patients come to us for brain fog, specifically, and Alzheimer's prevention.
CHAKRABARTI: Lisa, I can't help but to, when I hear you talk about the protective power of these reproductive hormones on the brain, right?
The increase and decrease in dendritic connections, the brain, the flux of it.
MOSCONI: You like that?
CHAKRABARTI: I love it. Neuroscience is absolutely fascinating and makes me feel even more proud of the female brain. But, and the fluctuation in brain energy. And when this happens in the, you call them the three P's of life, right?
MOSCONI: Yes.
CHAKRABARTI: Puberty what's the next one? Peri?
MOSCONI: Pregnancy.
CHAKRABARTI: Pregnancy and perimenopause?
MOSCONI: Perimenopause.
CHAKRABARTI: Yeah. But I can't help but to think, let's say in an evolutionary, from an evolutionary mindset, that you're also talking about times in a woman's life that are really intimately tied to reproduction, right?
MOSCONI: Yes.
CHAKRABARTI: Because you talked about during pregnancy, a lot of the surge in these hormones. It makes sense that a woman's brain would want to be super powered and protected during pregnancy.
And the reason why I point that out is, do you think one of the reasons why there has been inadequate study of menopause and the brain, or even as we heard our listeners at the beginning of the show say, people just don't even want to talk about it, is because from this, I guess, psychological perspective, that when you enter menopause as a woman, you're also exiting a definitive period of life where you can bear a child if you want to, right? So you've exited the period of time where you can bring forth life into this world. And so therefore, on a species level, you've exhausted your youthfulness.
And do you think that's kind of part of why there's been, you know, almost a deliberate scientific ignorance of wanting to study menopause more?
MOSCONI: Yeah, sure. I think in medicine we're a little bit penalized as women by this framework that I refer to as bikini medicine, which is really how historically medical professionals and scientists alike truly believed that women were essentially smaller men.
With different reproductive organs. But then, those differences aside, so if you just consider those body parts that fit under a bikini, that's saying that, from a medical perspective, what makes a woman are specifically her breasts and ovaries and nothing else. And medicine is based on this framework and neuroscience is based on this framework and it really all comes down to Darwin.
The father of modern biology, who very specifically said, the whole point of evolution is to have kids. Once you can no longer have children, then from an evolutionary perspective, you should just not stay alive. And that's very interesting if you're a man, because men are fertile through their 80s, right?
70s and 80s. But obviously, it does not apply to women. So there's been a push in evolutionary biology to really append this possibly faulty notion, by considering that evolution doesn't have to be as misogynistic as those who study it, right? Maybe there's something about women that make us valuable.
CHAKRABARTI: Beyond procreation.
MOSCONI: Absolutely. Which, anyone, I can tell you, it's just so obvious, but there's a hypothesis called the grandmother hypothesis. That states very clearly that for a it is actually more advantageous to stop being fertile at some point in your life and stay alive.
Because the chance of dying from childbirth are much higher the older you are, and also direct risks to the offspring with older parents. So it's better in some ways to no longer being able to have children but remain alive to help your daughters have children themselves. In this way you're still passing on your genes to the next generations. You just don't do it directly yourself, but you do it via your daughters and sons.
And that's a wonderful way to think about aging in general, if you think about grandmothers as evolutionary superheroes, in a way, who really stepped in to save the day. And this is especially important for our species because something that we really don't talk about is that menopause is a gift, is a blessing, the ability to outlive menopause is very unique in biology.
If you think about it. On the entire planet, there's only four animal species where the females are able to live after menopause. Women, thank goodness, some whales, some elephants, and the Japanese aphid, which is a bug. Aside from that, all other species die soon after menopause.
CHAKRABARTI: Isn't that fascinating?
MOSCONI: Yeah, I think it is.
CHAKRABARTI: Wow, okay. Lisa, stand by for a moment, because when we come back, I want to dig a little deeper with you about more of the why does menopause happen, and again, what happens in the brain, and then of course we'll get to that big question of hormone replacement therapy and your thoughts about it. We'll be back.
Part III
CHAKRABARTI: Lisa, I was going to actually get straight to the HRT question, but then suddenly it occurred to me over the break that of the four species that you say outlive the phase of life of menopause humans.
Elephants.
MOSCONI: Killer whales.
CHAKRABARTI: Is it specific, only killer whales?
MOSCONI: Yes.
CHAKRABARTI: Okay. Okay, just so humans.
MOSCONI: Killer whales. Narwhals.
CHAKRABARTI: So humans, narwhals and orcas and maybe some other whale species. Elephants, love them.
MOSCONI: One type of elephant.
CHAKRABARTI: Only one type. Which one?
MOSCONI: Yeah. The Asian.
CHAKRABARTI: The Asian, and not the African elephant?
Oh my god. Okay, so we could do a whole hour on just that. And then the last one, which I just did a double take. Did you actually say Japanese aphids?
MOSCONI: I did.
CHAKRABARTI: I didn't even know insects menstruated or had menstrual cycles. They don't.
MOSCONI: They don't menstruate. It's more like at some point they no longer are reproductive.
CHAKRABARTI: Oh, okay. Okay. My whole understanding of the insect kingdom was like, it was going to, or the insect phyla, was going to just blow up. So after their reproductive phase, these aphids live.
MOSCONI: Okay. Yes.
CHAKRABARTI: That's still amazing.
MOSCONI: They turn into a kind of spiky thing as they go through menopause.
It's really just do not touch me.
CHAKRABARTI: Oh, I love that. So I do want to hear a little bit more about more of the sort of, Why do you think, why does this happen? again. And we can talk about the brain connection here, because one of the answers you gave for the why of menopause was that just for humans, being pregnant later in life is much more dangerous for the woman are there any other answers why's of menopause?
MOSCONI: I think there are many ways menopause really needs to be researched in greater detail. But I think from a neurological perspective is also a good thing that's happening to us. Because so we are born with this neuro endocrine system that connects the brain with the ovaries and is very expensive to have it. Metabolically speaking.
It's a lot of neurons that need to be able to activate a menstrual cycle, activate a pregnancy, help you sustain a pregnancy. Once you go through menopause, you no longer need to get pregnant. All those neurons, all those connections, are no longer necessary. So menopause, this is my own personal hypothesis to be fully confirmed.
But as a neuroscientist, the way I'm thinking about it is that menopause is a biological clue for the brain to shed some neurons that are no longer needed and get leaner and meaner, if you will. There's a whole rewiring that takes place in the menopause brain that is in part about probably just getting rid of the neurons you no longer need. Although that, of course, creates some glitches. Changes in body temperature, changes in mood, and changes in memory, and changes in sleep.
But at the same time, this rewiring seems to be happening for a good reason, which is to really prepare women for the next phase of life, for the non-reproductive phase of life, that can be just as productive. And menopause seems to be associated with some good changes from a neurological perspective. Where women gain in empathy and emotional control, which are two very important factors to sustain happiness long term.
So one of the most interesting and surprising things that I come across about menopause is that postmenopausal women tend to report greater life contentment. And greater happiness over time, as compared to younger, premenopausal women, but mostly as compared to themselves before they went through menopause.
CHAKRABARTI: Yeah.
MOSCONI: I think this is a gift. Can be a gift.
CHAKRABARTI: It sounds wonderful. I presume there's a lot of confounders there, in terms of being able to say that's a pure causation, but the rewiring of the brain, though, it sounds a whole lot like the neural pruning that goes on for young kids when they're like, what, five, six, seven years old.
MOSCONI: And puberty. That's what happens to puberty and pregnancy. That's exactly what happens, that the brain sheds a lot of neurons. You lose gray matter volume at both puberty and pregnancy.
CHAKRABARTI: But isn't the thought that, I'm thinking of the neural pruning in young children, that it's not a negative thing, it's just the brain clearing out sort of the connections that it doesn't need any more in order to make the rest of the brain more effective and efficient.
MOSCONI: Exactly. That's exactly right. And there's reason to believe that something similar may be happening during menopause as well.
CHAKRABARTI: Okay.
MOSCONI: Just don't think about it that way, because everything about menopause is seen as doom and gloom. All the research on menopause is about looking at the downfall, looking at all the problems and the symptoms and finding a cure.
And we may be missing out on the positives that this transition brings. Earlier in the show I was trying, I was sympathizing with our listeners and calling their symptoms, it sounded like a neural apocalypse to me, so I'm going to take that, I'm going to take that back.
MOSCONI: No, but it feels like it, it sounds like it, it feels like it.
I think, see, this research is not to discount the symptoms and the challenges that women experience. It's more about putting it, putting everything in context, because if you understand what's happening in your brain and that there's a reason for it, it's a means to an end. At the end of the day, that gives you more agency and makes you feel more in power and more in control of your outcomes.
And I think that's really important. So on one hand, first of all, we're not making things up. It's not all in your head. You're not going crazy. These are real symptoms. Your brain is in fact changing, right? And then once we acknowledge that, we also understand that there are solutions and there are things that one can do to feel better and to avoid suffering. Menopause is this unique scenario in medicine where silent suffering is not only accepted, it's actually recommended or encouraged.
CHAKRABARTI: Yeah.
MOSCONI: And that is insane. All women go through menopause and over 85% of women experience brain symptoms during menopause and beyond.
CHAKRABARTI: Well on that note I have to turn back to our listeners because we also asked folks. Okay. So what do you do to treat your symptoms of menopause and silent suffering, that came up. And so here's what some of our listeners said.
(LISTENER MONTAGE)
RACHEL STARR: Kinda gritting my teeth and bearing through it.
ANDREA HARDY: I did finally find a perimenopausal support group.
BRIGETTE DINEEN: My nurse practitioner suggested Gabapentin and that has just been a lifesaver for me with the hot flashes.
PAM: Exercising on a regular basis, treating my body more healthy.
LILA ANNA: Started natural hormone treatment, I'm my old self again.
PAMELA: Instead of estrogen pills, they prescribed this cream. You rubbed it on your thighs. It helped so much.
AMY JACKSON: It's completely changed my life. My brain fog is gone. There's no more weird heat sensations.
Listeners Rachel Starr in Watertown, Massachusetts; Andrea Hardy in Portland, Oregon; Brigette Dineen in Lakewood, Ohio; Pam Curativo in Bar Harbor, Maine; Lila Anna in Columbia, South Carolina; Pamela in Maine; and Amy Jackson in Wake Forest, North Carolina.
Lisa, I think that one of the things that really jumps out at me is the completely spectacular variety of treatments that women turn to. What do you make of that? What does it tell you about the state of medicine and medical treatments around menopause?
MOSCONI: Yeah, it tells me a couple of things. The first thing that comes to mind is that Hormone Replacement Therapy, HRT, which is now called Menopause Hormone Therapy or MHT, is actually the first line of treatment for symptoms like hot flashes and night sweats.
But a lot of women do not choose that option, because of fears around breast cancer or other risks that have been a little bit exaggerated in the media. Almost 20 years ago. And HRT has been really suffering from this bad rep. It has been very hard to resolve in some way.
CHAKRABARTI: I have to jump in here because I don't think it was just a little bit exaggerated.
MOSCONI: Okay. I'm never sure.
CHAKRABARTI: No, you don't have to step lightly around that. It was one of those pitfalls that the media frequently falls into about, there's one finding in one study, for example, and no one reads about the internal relative risks that are revealed in that study.
And they just say, "Oh, look, it found that it increases your risk of breast cancer." And that's the headline that gets everywhere. And millions, thousands, hundreds of thousands, of millions, I don't know how many women, decided not to do hormone treatment. After that.
MOSCONI: Yeah, just went cold turkey, which is also just as unfortunate in some ways.
Yes, but what we know now about Hormone Replacement Therapy is that in 2022, which is just a year ago, just a little over a year ago, professional societies reviewed all the available evidence and determined that a change in guidelines was appropriate. So 2022 was a big year for HRT.
Where we now understand that for most women younger than age 60, or at least within 10 years of the final menstrual period, Hormone Replacement Therapy is safe to use, and the benefits typically outweigh the risks.
And this is in the guidelines, the approved official statements of the North American Menopause Society. Anyone can look it up.
CHAKRABARTI: Lisa, can I just jump in here because this is exactly what Dr. Jan Shifren from Massachusetts General Hospital told us. And I want to just get her thoughts in here from the perspective of an OB/GYN endocrinologist.
So when we did ask her, should you, shouldn't you, about HRT, here's what she first said.
SHIFREN: If you are basically healthy at the menopause transition, typically under age 60, and you're having bothersome hot flashes, the benefits of treatment for most women like you will really outweigh the risks.
CHAKRABARTI: So that's exactly what you just said, Lisa, but then, any good doctor will never tell you that anything is either 0% or 100% effective, that's why they talk about benefits outweighing the risks.
But Dr. Shifren also said there are some conditions that may warrant not using HRT or MRT, as you called it, such as if a woman has breast cancer, endometrial cancer, heart disease, blood clots in the legs, stroke, and those conditions mean don't use HRT. And then she also acknowledged there are some risks.
SHIFREN: What I always say to my patients is I'm going to share the risks and don't panic. So when we look at some of the published studies, in general, for women over age 50, menopausal hormone therapy has been associated with increased risks of heart disease, stroke, clots in the legs and lungs, gallbladder disease, and breast cancer.
And in women over 65, with cognitive decline and dementia. And that sounds terrifying.
CHAKRABARTI: But she says you shouldn't be terrified because this language associated with increased risk. You hear it all the time in things like pharma ads. But an association with increased risk doesn't necessarily mean the chances of a bad outcome jump from something small to something enormous.
In fact, Dr. Shifren told us that for women under the age of 60, the individualized risks actually change very little.
SHIFREN: We saw minimal, if any, increase in heart disease risk. The risk of stroke was increased very slightly, but women under 60 who are healthy are at incredibly low risk for stroke. There is a slight increased risk of breast cancer in women with a uterus who take estrogen and progestogen for more than four to five years, but it's a slight increased risk.
To help put that risk into perspective, the relative risk of breast cancer after four to five years of estrogen and progestogen use for a woman over 50 is about the same increased risk as having two alcoholic beverages a day or having a high weight.
CHAKRABARTI: So that's Dr. Jan Shifren, Director of the Midlife Women's Center at Massachusetts General Hospital.
Now, Lisa, this hour has absolutely flown by, and we only have a few minutes left. You spend quite a bit of time in the book also talking about, first of all, no, you're not imagining it. It is real. There are major changes going on in the brain due to that absolutely fascinating neural endocrine system.
Hormone replacement therapy for women under 60 can be a first line treatment for symptoms, but you also talk about other things that women can and should do in their lives as a whole, in order to ease this transition to this next phase of life. Can you talk about some of those?
MOSCONI: Yes. Happily. Very happy to. And I would say that I think the range of treatment should really reflect women's not just risks and needs, but also preferences. Many women prefer to navigate menopause naturally, which is a strange word, but without taking medications, and that is perfectly fine. And there are many lifestyle adjustments that one might want to consider that are not just helpful for menopause, but also for brain health as a whole.
And these include chiefly physical activity. Regular physical activity, healthy diet, stress reduction, really important, sleep hygiene, avoiding environmental toxins, intellectual stimulation and lifelong learning, and regular medical checkups.
CHAKRABARTI: These all sound like things we should be doing throughout our entire lives.
MOSCONI: Yes, and I think what's interesting is to tweak them towards your need for menopause, if you would like. Like for exercise, cardiovascular exercise, like running, jogging, skipping rope and whatnot, seems to be really helpful for things like hot flashes and brain fog. But strength training seems to be quite helpful for mood, as well. Whereas exercises like yoga, Pilates, Tai chi are more helpful for sleep and stress reduction.
So it's interesting to know that different types of exercise can help you more with one symptom over another. Like for diet, there are so many diets out there, but the plant forward diet is the only one so far that's been shown to be associated with better outcomes in menopause.
So fewer hot flashes, less mood swings, better sleep and better brain health.
CHAKRABARTI: You also talk about the power of a positive mindset. We've got about 30 seconds left. I'd love for you to close with that thought.
MOSCONI: Yes. So the symptoms of menopause are not universal. There are women in different countries who do not even have hot flashes, which is important. Because it tells you that perhaps there's also a cultural component to menopause, or a psychological component, or a mindset component to the way we experience menopause.
And what's interesting is that in cultures where menopause is not dreaded, but people actually look, women really look forward to being post-menopausal because they gain in social status, or they have more freedom, or they're free from having cramps during their menstrual cycle. The whole experience of menopause is better, and the symptoms are less severe.
So there is something that our brain is a powerful organ and if we can just stay positive and feel empowered that we can make it through menopause. There's nothing to fight, there's nothing to fix. It's a phase. We need support, no doubt, but we can do it. We can do it. And I think there's power in that.
CHAKRABARTI: Lisa Mosconi, I hope this conversation has helped many women feel empowered. She's a neuroscientist and author of “The Menopause Brain." Thank you so much for joining us today.
MOSCONI: Thank you so much for having me. It was a real pleasure.
This program aired on February 28, 2024.

