Advertisement
Boston Doctors Confront Another 'Terrifying' COVID-19 Reality: Patients Dying Alone
Resume
With the lives of many Americans hanging in the balance, hospitals are doing all they can to limit the spread of the coronavirus. One change: restricting visitors.
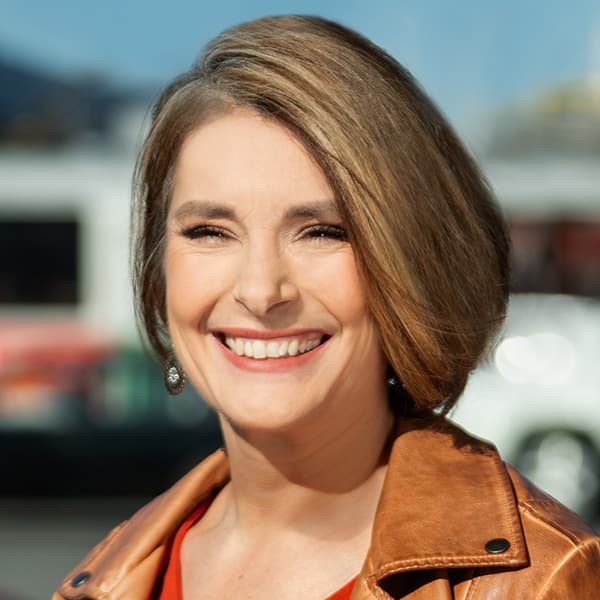
That change has left one critical care doctor, Dr. Daniela Lamas at Brigham and Women's Hospital in Boston, reckoning with the fact that her patients now have to suffer alone. She wrote about her experience and spoke with Radio Boston.
Interview Highlights
On how she's thinking about her patients having to suffer in solitude
"I wrote the [New York Times] piece as a way to begin to process what I could tell at the time and have only seen more things would be our new reality ... Clearly, this is an experience that we can all imagine what it might be like to be in, or be afraid of. This idea of loneliness and isolation is something that we're facing in our everyday lives. The idea that we have to face it when we're sick, [that] our loved ones would have to face it, is terrifying."
On what that has meant for her patients at Brigham and Women's Hospital
"I was [working yesterday] and told a parent that her adult child was getting sicker, who might need to intubate. She was just miles away and could have gotten in an Uber or driven herself to the hospital, but [she] could not come. I heard that she had real panic in her voice [and] I wasn't able to help her at all. I wasn't able to say, 'Why don't you come?' I put her on speakerphone with her son and they talked. Maybe that was something, but it wasn't enough. It wasn't what she wanted or needed. These are small tragedies that are being played out dozens of times in every hospital right now."
On what more doctors can do for their patients right now
"I've gained the understanding that we can't pretend that ... a phone call might be just as good [as an in-person visit]. It's not just as good. But ... we can do small things, [like] putting our phone on speakerphone to allow a family member to speak to somebody who may be intubated [even if they can't respond]. I think just being aware of what our patients have lost, what their families have lost and what we as their providers are losing and acknowledging, that this is one step."
On the long-term impacts of this isolation for patients, families, and providers:
"In the ICU, we meet people when they are often not awake and we don't know who they are as people, who they were before this event, who they ideally will be afterward. Families are the ones who give us that. They give it to us in an iterative fashion. They give it to us as they stood at the bedside over conversations. They give it to us by being present on our daily rounds. So, I think that we lose that ...
"In a longer-term way, I do worry about the effect of this separation [and isolation] on psychiatric outcomes for families [and] for patients who've survived this crisis."
This article was originally published on March 31, 2020.
This segment aired on March 31, 2020.